Today, we're zooming in on a specific yet vital part of healthcare: the chest pain SOAP note.
If you've ever wondered how clinicians efficiently document those potentially life-changing patient encounters, especially when chest pain is a concern, you're about to find out.
This blog is your ultimate guide to understanding and mastering the art of the chest pain SOAP note.
We're going to cover:
- The ins and outs of what a chest pain SOAP note is and why it's indispensable
- A detailed walkthrough on how to write a chest pain SOAP note
- Examples of chest pain SOAP notes to illustrate best practices
- The tremendous role of AI tools, like Lindy, in streamlining the creation of chest pain SOAP notes
Let's dive right in!

What is a SOAP note and why do you take them?
A SOAP note is a structured way of documenting a patient encounter. It stands for Subjective, Objective, Assessment, and Plan.
You take SOAP notes to have a systematic way of organizing information about your patient.
- The Subjective section describes the patient’s symptoms, like chest pain in this case.
- The Objective section includes your exam findings, vital signs, and test results.
- The Assessment is your interpretation of the subjective and objective data. What do you think is going on with the patient?
- Finally, the Plan details what you’re going to do for the patient.
SOAP notes provide a structured format for organizing information about your patient so you can provide the best care.
Plus, they also serve as a medical-legal document about what was done during the visit.
How to write a chest pain SOAP note
When a patient complains of chest pain, it's absolutely essential to get the details documented properly in a SOAP note.
As we said, the S stands for Subjective information directly from the patient.
Ask open-ended questions about the pain like:
- When did the pain start?
- How would you describe it? Sharp, dull, crushing?
- Does anything make it better or worse?
- Have you had chest pain before?
Record the patient's answers word-for-word.
For Objective data, note vital signs and the results of a cardiac exam. Listen for abnormal heart sounds and check for swelling in the legs. Then, review any test results or scans that have already been done.
In your Assessment, you have to determine if the chest pain is likely cardiac or non-cardiac in origin based on the information gathered. For cardiac chest pain, it could be acute coronary syndrome like angina or heart attack. You'll want to rule these in or out.
Finally, the Plan details what should happen next. This may include admitting the patient into an ICU, ordering further tests like an EKG, cardiac enzymes or stress test, or scheduling a cardiology consult. You should also include any medications given.
When documenting a SOAP note, be thorough but concise. You’ll want to focus on clinically relevant details and avoid repetition. Type or dictate notes into the patient's electronic health record as soon as possible while the information is still fresh in your mind.
Two examples of SOAP notes for chest pain patients
Need some real-world examples to get started? Here are two chest pain SOAP note examples to get you on the right track.
Example 1 - 76-year-old male
Subjective: 76-year-old male with a history of diabetes, hypertension, and sleep apnea presents with chest pain that began yesterday.
He describes the pain as sharp, followed by a dull ache. He has a known right bundle branch block and occasional premature ventricular contractions.
Objective: Vital signs are normal. Physical exam shows no abnormalities. EKG shows normal sinus rhythm with a right bundle branch block, similar to previous EKGs. Labs show an elevated glucose of 180 mg/dL but are otherwise normal.
Assessment: New onset chest pain in a patient with known coronary artery disease risk factors.
The pain could represent stable angina, but acute coronary syndrome cannot be ruled out based on the information available.
Plan: The patient was admitted to the hospital for further evaluation and management. Cardiac enzymes were trended, and stress testing was planned to evaluate for inducible ischemia. The patient was placed on aspirin, beta blocker, statin, and nitroglycerin as needed for chest pain.
Example 2 - 67-year-old female
Subjective: 67-year-old female with a history of hyperlipidemia presents with intermittent chest pain over the past week. The pain is dull, pressure-like, and lasts for 30-60 minutes.
It’s occasionally associated with nausea but no other symptoms. She denies any previous episodes of similar chest pain. Her only medication is atorvastatin.
Objective: Vital signs and physical exams are normal. EKG shows normal sinus rhythm without ischemic changes.
Assessment: The patient's presentation is concerning for angina pectoris due to underlying coronary artery disease. However, other causes of chest pain such as gastroesophageal reflux disease or chest wall pain cannot be excluded based on the information provided.
Plan: The patient was referred for an exercise stress test to evaluate for inducible ischemia. She was counseled to go to the emergency room immediately if her pain became more frequent or severe, radiated, or was associated with other symptoms.
She was also provided education on risk factor modification. Follow-up with her primary care physician was recommended after the stress test results were available.
Streamlining your chest pain SOAP notes with AI
We’re going to tell you something you probably know already: Crafting detailed notes for each patient will take up a significant portion of your time.
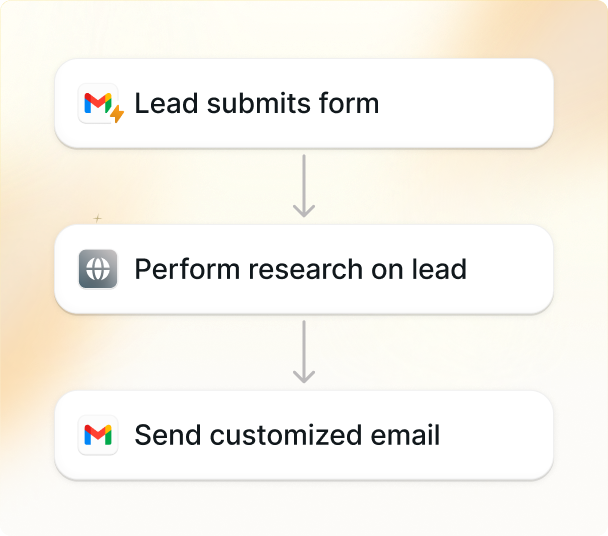
This is where AI tools like Lindy can take a load off your back.
Here are some ways you can use Lindy for great chest pain documentation:
Subjective (S):
- Voice dictation: Describe the patient's history, symptoms, and timeline of events using voice dictation, and Lindy will transcribe it into the S section in real time.
- Pre-built templates: Use specific templates to capture key details like location, duration, character, radiation, and aggravating and alleviating factors.
- Customizable prompts: You can add custom prompts to get specific information relevant to your practice or patient population – like past medical history or risk factors.
Objective (O):
- Immediate EHR connection: You can easily plug Lindy into your EHR to auto-populate vital signs, physical exam findings, and laboratory results in the O section.
- Dictate: Use voice dictation to give detailed descriptions of physical exam findings and any other relevant observations.
- Imaging integration: Lindy also plays nice with imaging tools to seamlessly include relevant reports and findings.
Assessment (A):
- Unobtrusive coding suggestions: You can use Lindy's suggestions for relevant ICD-10 codes based on the patient's presentation and diagnosis.
- Differential diagnosis: Use Lindy's access to clinical decision support tools to explore possible diagnoses based on the information you’ve gathered.
- Collaborative tools: You can share preliminary diagnoses and assessments with colleagues safely and securely within the platform for real time feedback and discussion.
Plan (P):
- Pre-built plan templates: Use templates specific to chest pain management, including diagnostic tests, medications, and treatment recommendations.
- Full customization options: Adapt the templates to fit your specific patient's needs and preferences.
- Patient education resources: You can access and share relevant patient education materials within the platform for even more patient engagement and understanding.
While technology has significantly improved many healthcare areas, documenting patient interactions is still as analog as ever.
AI tools like Lindy are changing that by enhancing and optimizing these time-consuming but important jobs.
FAQs
Do I need to take SOAP notes for every patient?
Yes, it’s best practice to take SOAP notes for each patient encounter. They provide a consistent way to document the details of a patient's condition and the care provided. SOAP notes allow you and other healthcare providers to get a quick overview of the patient's history and plan the best course of treatment.
How often should I review and update SOAP notes?
You should review and update SOAP notes for each patient at every visit. Add details about the current visit, update the assessment and plan sections based on the latest information. It’s also a good idea to review notes from past visits to identify any changes or trends in the patient's condition over time.
What should I include in the subjective section?
The subjective section should document the patient's symptoms, medical history, and any concerns or issues from their perspective. Be sure to include details about:
- The onset and duration of current symptoms
- Severity and quality of symptoms
- Any factors that improve or worsen symptoms
- Medical history including diagnoses, surgeries, hospitalizations
- Family medical history
- Medications and allergies
- Social history including lifestyle factors that could impact health
Do I have to use a particular format for SOAP notes?
There’s no single required format for SOAP notes, but most organizations have their own guidelines. The most important thing is that the notes are clear, concise, and contain all the necessary information about the patient's condition and care. A logical flow like: Subjective → Objective → Assessment → Plan works well. Within each section, be consistent in how you organize details and the level of detail you provide.

Conclusion
We've covered a lot of ground here! From understanding what SOAP notes are and why they matter, to walking through examples and tips, you're now equipped to start taking effective SOAP notes in your clinical practice.
As we wrap up, remember that while SOAP notes do take time, they provide essential documentation and help you get all-important details during patient visits.
So, get them right!