I tried the top 5 AI medical documentation tools in 2026, and the differences were huge.
Some were clunky. Some couldn’t handle accents or medical terms. And a few felt more like note-takers than actual assistants.
But one tool stood out for speed, accuracy, and real workflow impact.
In this guide, I’ll break down what worked, what didn’t, and which AI medical documentation tool is actually worth your time.
What is an AI Clinical Documentation?
AI clinical documentation refers to the use of artificial intelligence to automate and improve the process of creating and managing medical records. This includes tools that can transcribe patient encounters, generate clinical notes, and analyze large datasets of patient information.
In plain terms, it’s designed to take the pressure off doctors and nurses by handling most of the documentation work automatically. When I started using these tools, I noticed right away how much smoother they made my workflow, especially during busy clinic days.
Best 5 Medical Documentation AI Tools
- Lindy: Best for real-time, high-speed documentation
- DeepScribe: Best for accurate notes with billing support
- Freed: Best for effortless setup and daily use
- Tali AI: Best for multi-device, flexible documentation workflows
- Suki: Best for coding, orders, and large teams
Key Terms You Should Know in AI Medical Documentation
1. Lindy: Best for real-time, high-speed documentation
What does it do? Lindy transcribes clinician-patient conversations into structured EMR-ready notes with smart task suggestions and scheduling tools.
Who is it for? Lindy is great for clinicians who want fast, accurate documentation with EHR integration.
Lindy is designed to feel like a high-performing clinical assistant, one that listens in real time, understands context, and helps clinicians finish documentation before they leave the room. It doesn’t just transcribe conversations, it actively generates structured, EHR-ready notes while surfacing smart suggestions during the encounter.
You can also integrate Lindy with the EHR to reference patient data and pre-fill relevant note sections, reducing repetitive typing and turning documentation into a quick review process.
As clinicians speak, Lindy can auto-draft referrals, flag mentioned labs, suggest follow-up actions, and adapt to the way each provider works, all without disrupting the flow of the visit.
With a range of customizable note templates and multilingual support, Lindy works across specialties and care settings. It continuously learns from a clinician’s speech patterns, abbreviations, and preferred phrasing to improve accuracy and personalization.
Built with HIPAA and SOC 2 compliance at its core, Lindy meets the highest standards for healthcare security and privacy.
Lindy also includes a built-in scheduling assistant that syncs with Google Calendar and other tools, helping teams manage appointment logistics without constant back-and-forth. It’s built to reduce charting time, cut admin work, and support clinicians through every stage of care.
Pros
- Lindy Academy for 24/7 support
- Multi-language support and privacy compliant
- Customizable note templates for different specialties
- Dynamic, real-time suggestions during conversations
Cons
- Feature set may feel too broad for simple use cases
- Some EHR systems may need setup assistance for integration
Pricing
- Free plan: Includes 400 monthly credits, up to 400 tasks, and a 1 M-character knowledge base, great for testing the basics or building your first agent.
- Pro ($49.99/month): 5,000 credits, 5,000 tasks, 20 M-character knowledge base, premium actions, phone call support
- Business ($299.99/month): 30,000 tasks, phone call automation, priority support, 20 M-character knowledge base
{{templates}}
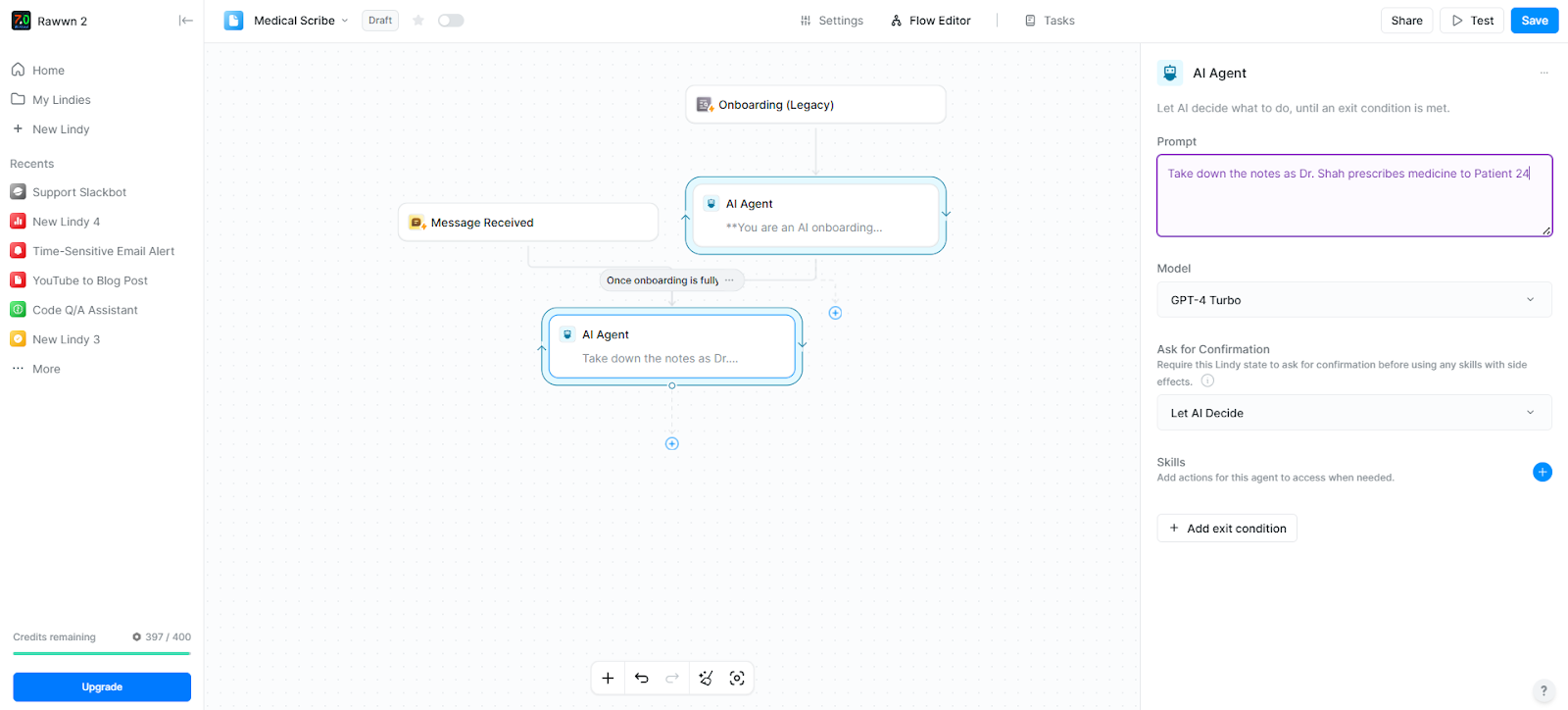
2. DeepScribe: Best for accurate notes with billing support
What does it do? DeepScribe transcribes real-time patient conversations into structured clinical notes.
Who is it for? It's best for physicians and specialists looking to automate their documentation without disrupting patient flow.
DeepScribe isn’t just another AI clinical documentation tool, it actually understands the rhythm of a real clinic.
What makes it stand out is how quietly it works. Once it’s on, it listens in the background during patient visits and uses its clinical notes software to build useful notes without interrupting the conversation. No need to trigger recordings or dictate anything after the appointment.
It’s not just dumping a transcript either. DeepScribe pulls out the clinically relevant parts, tailors them to your specialty, and formats them the way you already write. It also suggests E/M codes and handles ICD-10 and HCC tagging behind the scenes. That coding support alone makes a noticeable difference in billing accuracy.
We also appreciated how smoothly it integrates with EHR systems. There’s no double entry or copy-paste, just a finalized note pushed straight into the chart.

DeepScribe even provides real-time access to key patient data, which comes in handy during follow-ups or chronic care management.
Pros
- Non-intrusive ambient recording
- Works across multiple specialties
- Smart E/M coding and tagging support
Cons
- No visible pricing info on their website
- Not ideal for clinics without stable internet
Pricing
Not publicly listed. DeepScribe operates on a custom pricing model, so you need to contact their sales team for a quote.
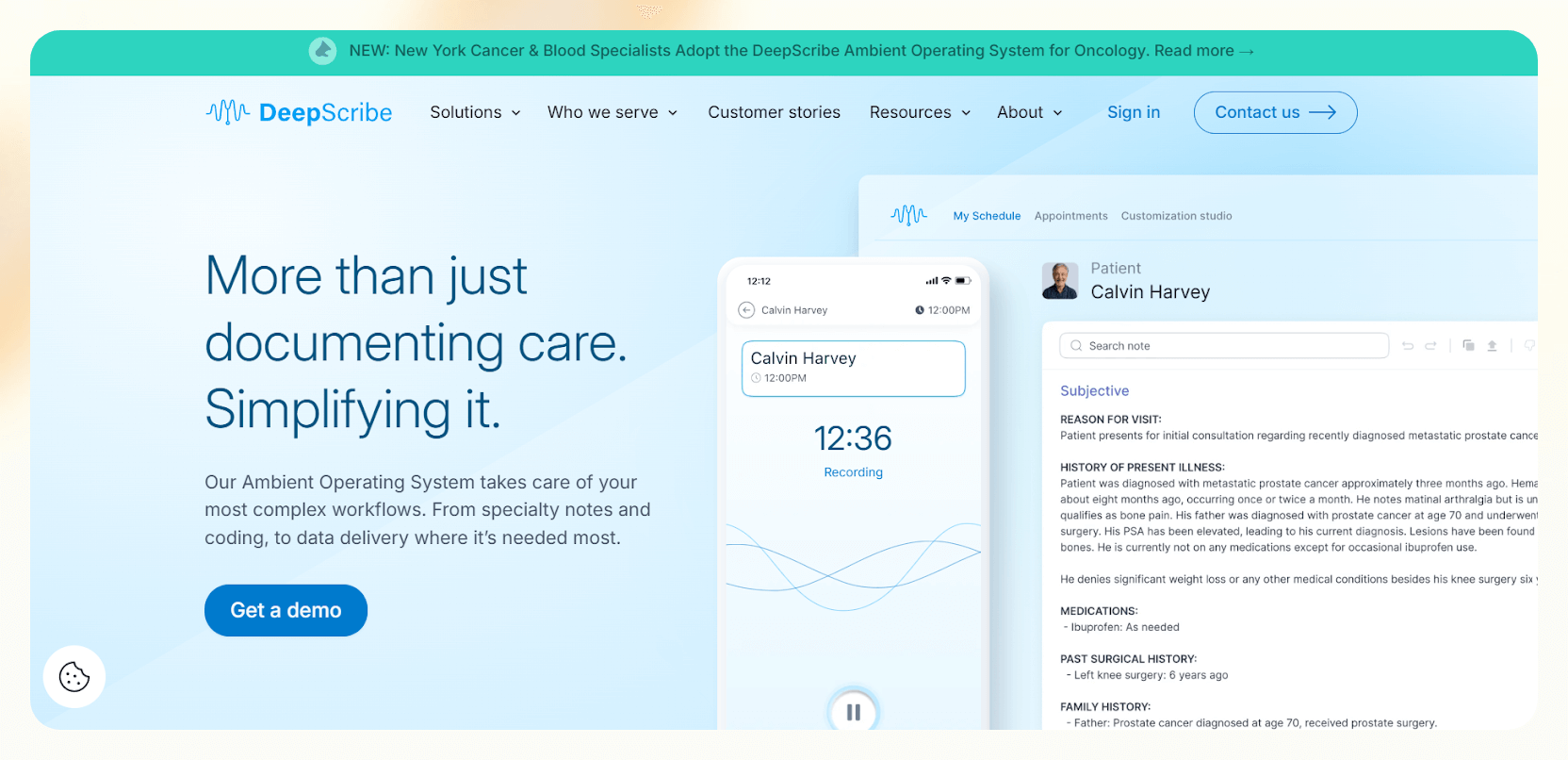
3. Freed: Best for effortless setup and daily use
What does it do? Freed captures and converts patient conversations into structured clinical notes in real time.
Who is it for? Ideal for clinicians who want a plug-and-play AI scribe without complex setups.
Unlike tools that require a full demo or training session, Freed lets you start documenting almost instantly. You hit record, see your patient, and by the time the visit ends, your SOAP note is ready. It is easy to use, works quietly in the background, and does not get in the way.
One of its most helpful features is “Learn My Format,” which allows the tool to adapt to your style of writing. Over time, it starts sounding more like you, whether you prefer shorthand notes, full sentences, or something in between.
You can also revise drafts using “Magic Edit,” get AI-generated summaries before each visit with “Smart Visit Prep,” and generate post-visit instructions with just a few clicks. These little things add up, especially on busy clinic days.
While solo users do not get direct EHR integration, exporting to text or PDF is smooth. Copying your notes into the patient chart only takes a few seconds, so it never feels like extra work.
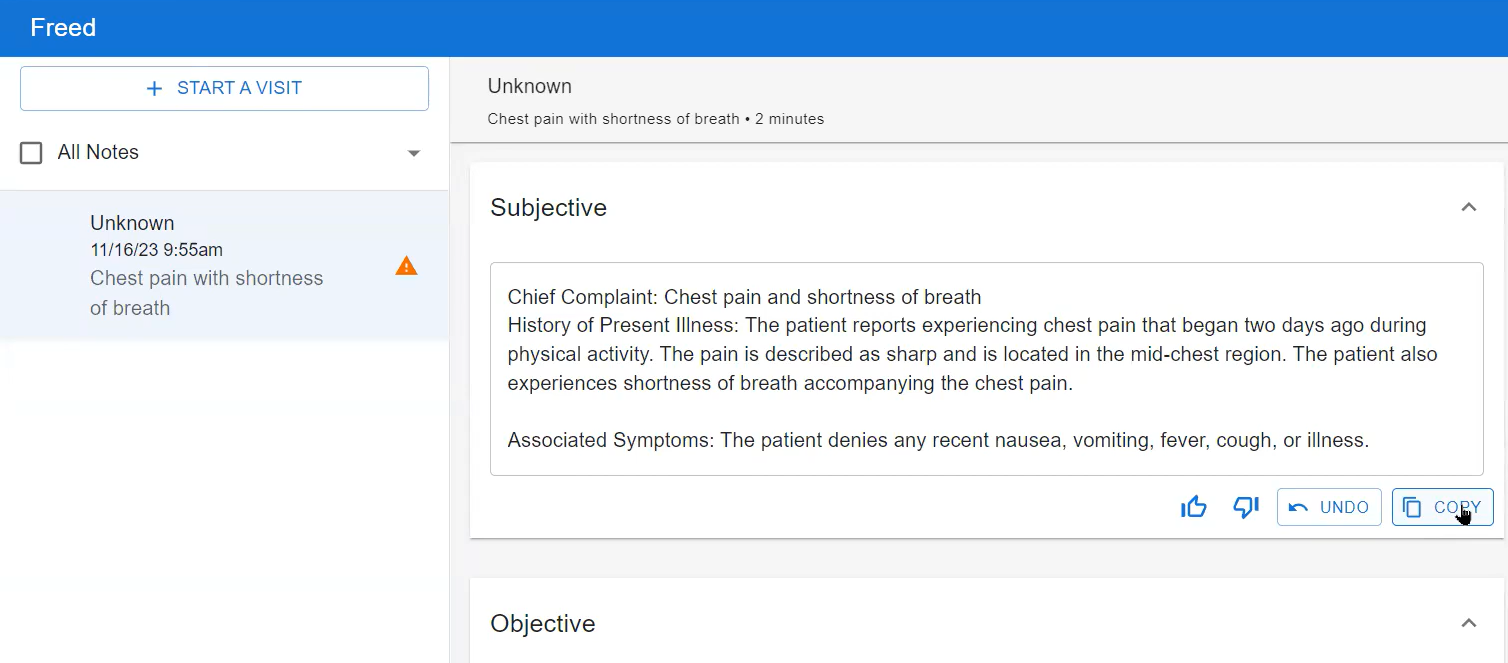
Freed also supports visit recording uploads, full visit transcripts, and a custom template builder, making it a solid option for physicians, therapists, and nurses alike. It covers a lot of ground without adding complexity, which is exactly what many clinicians need.
Pros
- Flexible export options (text, PDF)
- Learns clinician phrasing with “Learn This Style”
- Fast note generation with no onboarding required
Cons
- Manual export slows down larger team workflows
- No coding support, which limits billing automation
Pricing
- $99/month with unlimited charting
- Custom plans for teams or group practices
4. Tali AI: Best for multi-device, flexible documentation workflows
What does it do? Tali AI captures patient conversations and clinician dictation to auto-generate medical notes directly inside your EHR.
Who is it for? It's ideal for providers who want full control over documentation across web, mobile, and desktop.

Whether you are working from a clinic, home, or on a telehealth call, Tali works across platforms, including web, mobile, and as a Chrome overlay inside your EHR. You can move between devices without losing functionality, which makes it a strong pick for clinicians on the go.
Tali supports both ambient scribing and voice dictation, and it handles varied speech patterns and accents surprisingly well.
The Smart Edit feature lets you revise notes using natural language instructions, translate them into over 25 languages, and even generate AI-powered patient instructions after each visit. You can also resume unfinished encounters, so no information is lost if you pause and return later.
The Chrome overlay is more than just a shortcut. It allows you to search medical questions, like drug dosages or clinical guidance, using trusted sources, and insert templated notes without switching tabs.
Templates themselves are fully customizable, so you can set your own headings, structure, and formatting rules.

It does not yet offer coding assistance or integration with vitals and lab systems, so it may not suit complex billing-heavy workflows. But if you want a fast, flexible documentation tool that adapts to your pace and platform, Tali is one of the most versatile options out there.
Pros
- Responsive across web, mobile, and desktop
- Chrome overlay enhances in-EHR note-taking
- Switches between dictation and ambient scribing
Cons
- Limited coding support compared to other tools
- Chrome overlay compatibility varies across EHRs
Pricing
Custom pricing via request
5. Suki: Best for coding, orders, and large teams
What does it do? Suki captures patient conversations and automates notes, coding, and orders within the EHR.
Who is it for? It's ideal for enterprise health systems and clinicians juggling complex workflows.
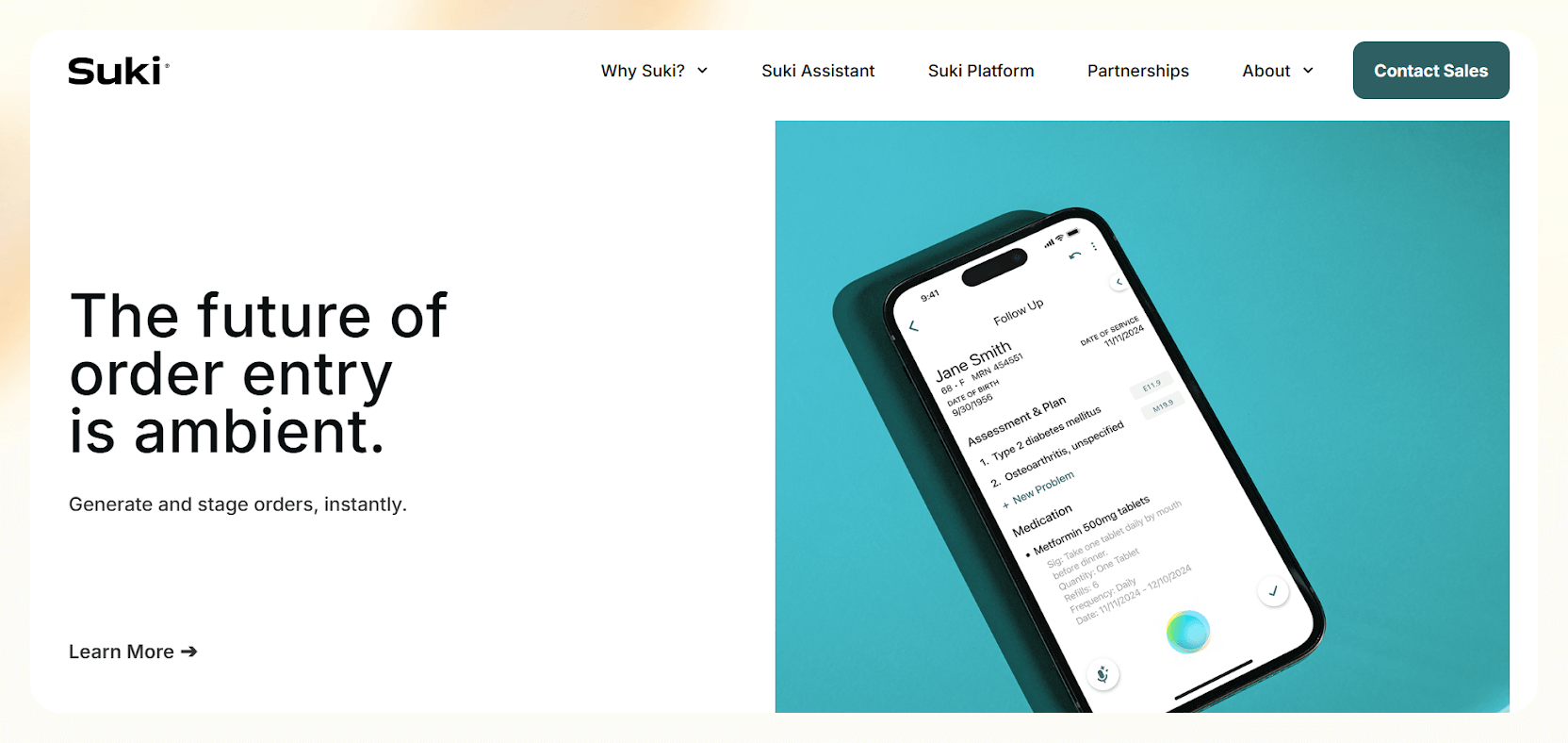
Using Suki feels like having a real assistant by your side. It listens, understands, and handles the full arc of clinical documentation, from drafting notes and suggesting ICD-10 codes to even staging medication orders during the visit.
For high-volume specialists and enterprise teams, that kind of automation saves serious time.
In testing, Suki pulled in vitals and diagnosis history on its own, then generated problem-based notes with accurate, context-aware coding suggestions. Everything was formatted and billing-ready without needing post-visit cleanup.
The built-in medical Q and A was surprisingly useful too. Ask a treatment question, and it pulls from clinical references to give a direct, reliable answer.
What makes Suki especially powerful is how it learns as you use it. Its speech recognition adapts to accents and clinical vocabulary, while machine learning personalizes your notes over time. It supports 99 medical specialties, works across Epic, Athena, and Oracle systems, and is backed by around-the-clock support.
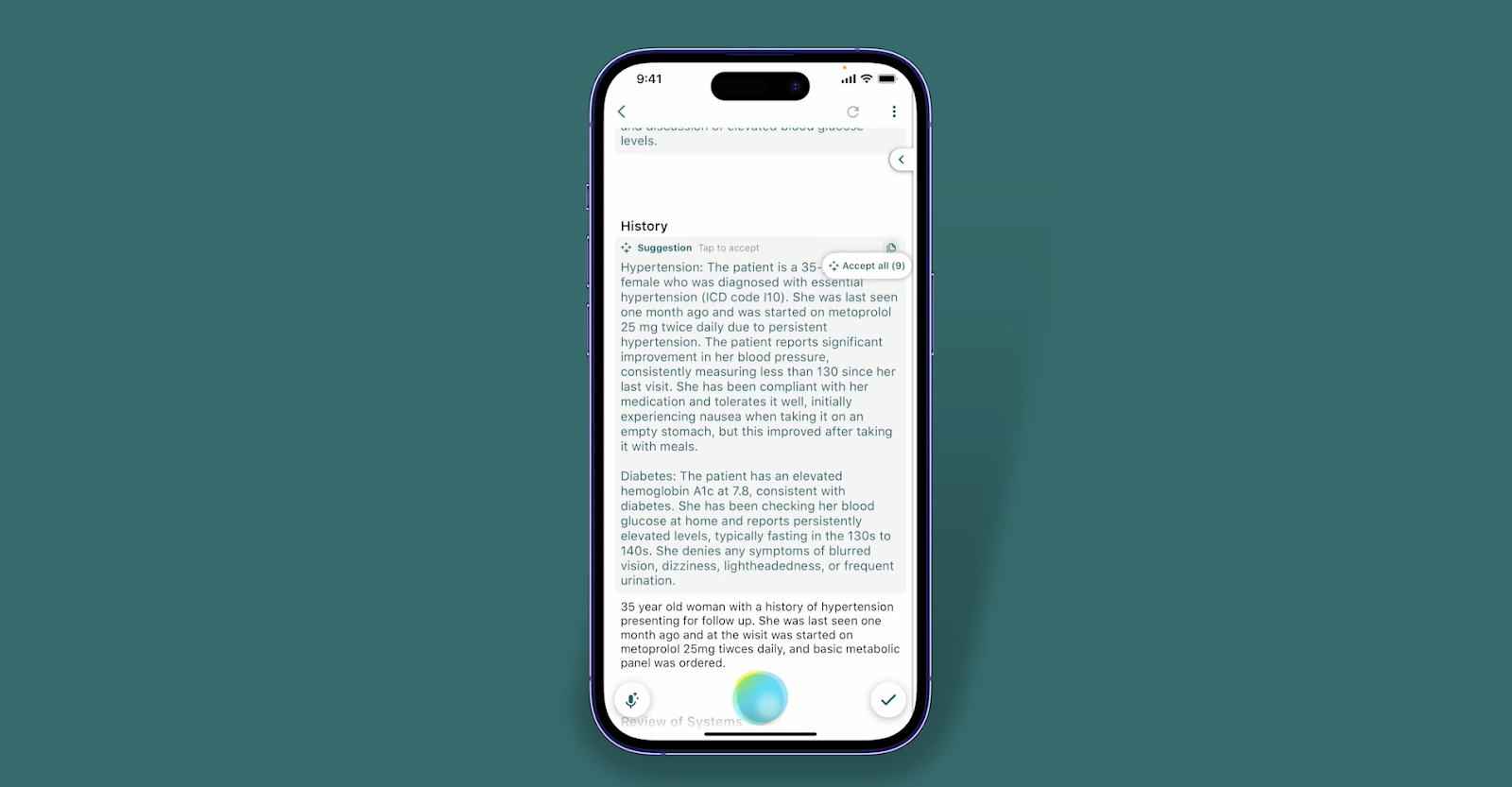
Suki is clearly built for scale. It is not aimed at solo providers, but in a team setting where speed, coding precision, and system integration matter, it stands out.
Pros
- Built-in medical Q&A for real-time reference
- Scales well across enterprise health systems
- Supports Epic, Athena, and Oracle integrations
Cons
- Enterprise focus may not suit solo or small teams
- Complex setup for clinics without EHR integrations
Price
Custom enterprise pricing based on deployment scale
How I Tested the Best Clinical Documentation Software
Great AI documentation software should feel like part of your clinical routine, not an extra step.
After testing dozens of tools, I focused on three things that actually matter:
- Reducing EHR time without creating more admin work somewhere else
- Fitting into a clinician’s workflow, whether in person, remote, or after-hours
- Accurately capturing patient-provider conversations, without needing constant corrections
To see which tools lived up to the promise, I ran each one through the same real-world scenarios and judged them on three key fronts:
Accuracy and clinical relevance: I used each tool during live or simulated visits and examined the output closely. Were the notes medically sound? Did they capture the right symptoms and treatment plans? I also checked how well they handled specialty-specific language and how much editing they needed.
Workflow compatibility and EHR integration: Good AI shouldn’t force you to change how you work. I tested each tool with major EHRs (like Epic and Athena), looked at overlays and syncing, and switched between dictation, ambient scribing, and templates to see how flexible they really were.
Speed, setup time, and bonus features: Some tools needed setup and training. Others worked right away. I tracked how long it took to get useful notes, how well they learned my phrasing, and which ones offered smart extras like ICD coding, referral suggestions, or scheduling support.
Not all AI scribes are created equal. Some are lightning-fast note-takers. Others feel more like full clinical assistants. This guide breaks down which is which.
{{cta}}
Lindy: The Best AI Medical Documentation
Lindy is the best AI medical documentation tool because it doesn’t just take notes, it manages the entire documentation workflow from start to finish. It listens in real time, generates structured clinical notes, fills EHR fields, summarizes patient history, and automates follow-ups like referrals or post-visit emails.
Whether in-clinic, remote, or across specialties, Lindy adapts to any workflow. It supports customizable templates like SOAP or H&P, integrates with tools like Slack and Google Docs, and works natively with major EHRs.
Try Lindy for free today! It's for clinicians who want accurate, adaptive, and end-to-end documentation without the overhead.
Frequently Asked Questions
1. How accurate are AI medical documentation tools?
The best tools are highly accurate, especially those using large language models and medical-tuned speech recognition. That said, most still require quick human review before final submission. Tools like Suki and Lindy offer clinician-controlled final edits.
2. Do AI tools work with all EHR systems?
Not all tools work with every EHR out of the box. Some (like Lindy and Suki) offer deep integration with major platforms like Epic, Cerner, athenahealth, and MEDITECH. Others rely on copy-paste or manual uploads. Always check integration options before committing.
3. Can these tools handle multiple specialties?
Yes. Most modern clinical documentation AI tools support dozens of medical specialties from family medicine and pediatrics to orthopedics and cardiology. Tools like Lindy support 99+ specialties and offer custom workflows for different clinical needs.
4. Is voice the only input method?
No. While many tools are optimized for voice, most also support typed input, manual edits, or a hybrid approach. Some (like Lindy) even work off calendar events or uploaded documents to generate notes.
5. Are these tools HIPAA compliant?
All top-tier clinical notes software and tools are HIPAA compliant and offer enterprise-grade security. Look for SOC 2 certification, end-to-end encryption, and clear data control policies. For example, Lindy only processes anonymized data for training and keeps clinicians in control.
6. What’s the difference between ambient documentation and regular dictation?
Ambient documentation runs in the background and captures conversations as they happen, no commands or dictation required. Dictation, on the other hand, requires you to speak your notes manually. Ambient tech (like Suki or Lindy) feels more natural and hands-free.
7. Are these tools also useful for nurses and other providers?
Absolutely. Many AI documentation tools are designed for use across roles, including nurses, physician assistants, therapists, and specialists. The benefits apply anywhere documentation takes up time and mental bandwidth.
8. How much do these tools cost?
Most vendors offer custom pricing based on team size and usage. Some, like Lindy, offer a free plan with 400 monthly tasks, while enterprise-level plans scale up to tens of thousands of tasks per month.


















.avif)
.avif)

.png)
%20(1).png)


.png)