Clinicians spend an average of 2.5 hours writing notes each day. This time can be spent doing better stuff while AI takes over. This guide will help you write clinic notes way faster so you can get back your time, and your life outside your job.
What Are Clinic Notes?
Clinic notes, or SOAP notes, are what doctors, nurses, and other healthcare professionals write to document interactions with patients. They contain information like symptoms, diagnoses, and treatment plans.

Why are Clinic Notes Important?
You should properly document patient encounters because it:
- Ensures patients get consistent care, even when switching doctors or clinics.
- Makes it easier to notice recurring symptoms or underlying patterns.
- Helps you stay on top of follow-ups, lab results, and next steps.
- Protects you legally by documenting every step of treatment.
- Keeps your entire care team on the same page.
What Do Clinic Notes Usually Include?
- Patient info: Name, age, date of visit
- Chief complaint: The main reason the patient came in
- History: Any relevant medical, surgical, family, or social history
- Symptoms: What the patient is experiencing
- Examination: What the doctor observed or examined
- Diagnosis: What the provider believes is wrong
- Treatment plan: Medication, tests, follow-ups, referrals
- Provider notes: Any additional observations, clinical reasoning, or instructions
Example:
Let’s say you visit for a persistent cough. A clinic note might look like:
- Chief complaint: Cough for 2 weeks
- History: No fever, non-smoker
- Exam: Clear lungs, no wheezing
- Assessment: Suspected mild viral bronchitis
- Plan: Rest, fluids, no antibiotics needed
How to Write Clinic Notes Using the SOAP Method?
The SOAP method offers a clear and organized system for documenting patient encounters. It's like a cheat sheet for crafting concise yet comprehensive notes.
Let's break it down step-by-step:
1. Capture the Patient’s Story (Subjective)
Document exactly what the patient tells you. This includes:
- Their main complaint
- Symptom descriptions (onset, location, duration, severity)
- Medical, family, and social history
- Any concerns or goals for the visit
How Lindy helps:
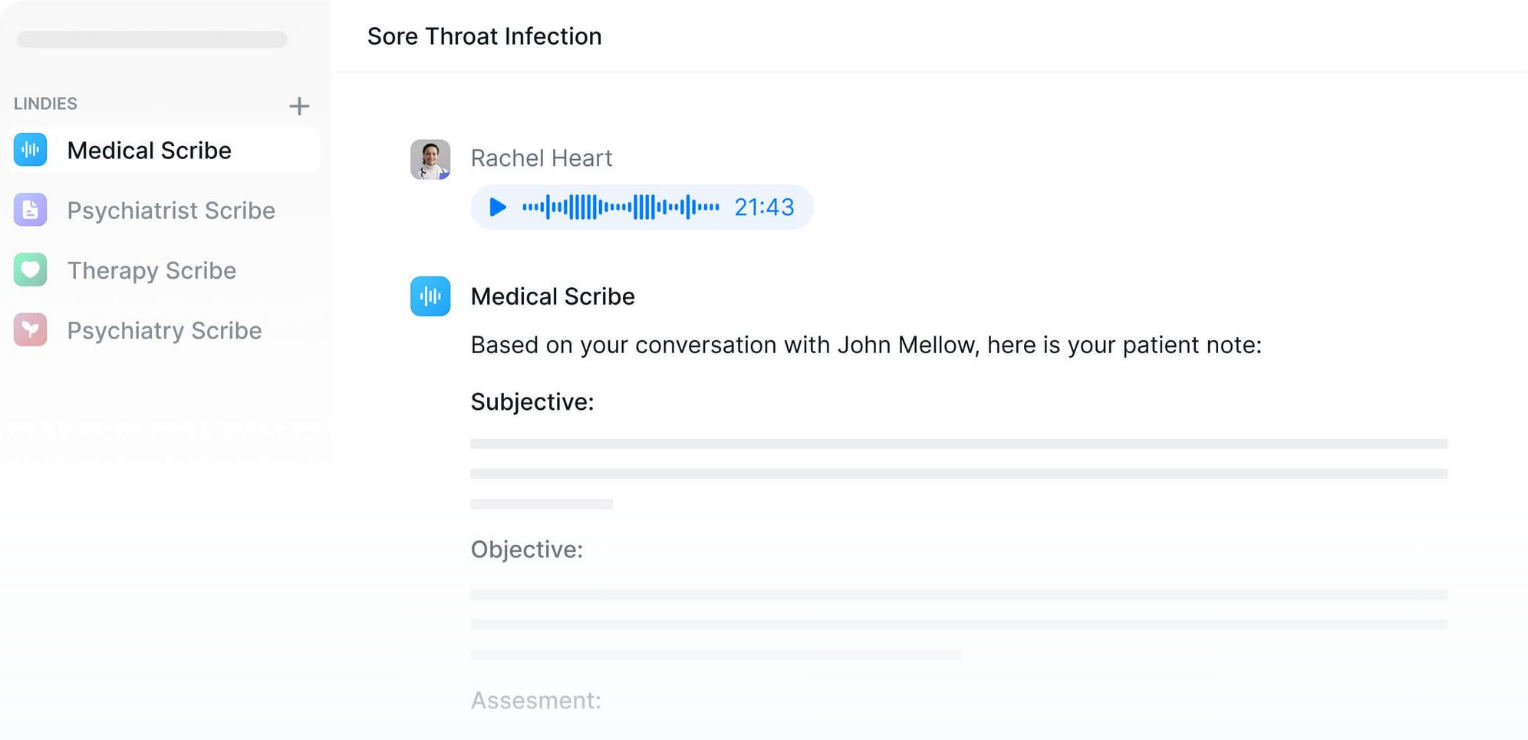
- Use Lindy to record live patient conversations or dictate immediately after the visit.
- Lindy’s AI transcribes and filters the dialogue, pulling only the relevant subjective content.
- It auto-tags key details like onset, duration, and symptom severity, saving you from manual entry.
Ask detailed questions but keep your notes clear and focused. Summarize only what’s relevant to the current visit.
2. Record What You Observed (Objective)
Write down what you see, hear, or measure. This can include:
- Vital signs (BP, HR, Temp, RR, etc.)
- Physical exam findings
- Lab or imaging results (if available)
- General appearance or clinical impressions
Stay factual and avoid assumptions. Just the observable evidence.
How Lindy helps:
- Dictate observations and Lindy turns them into structured bullet points or prose.
- If synced with your EMR or devices, Lindy can auto-import vitals and labs.
- Use shortcuts or templates like “Lindy, add normal cardio-respiratory findings.”
{{templates}}
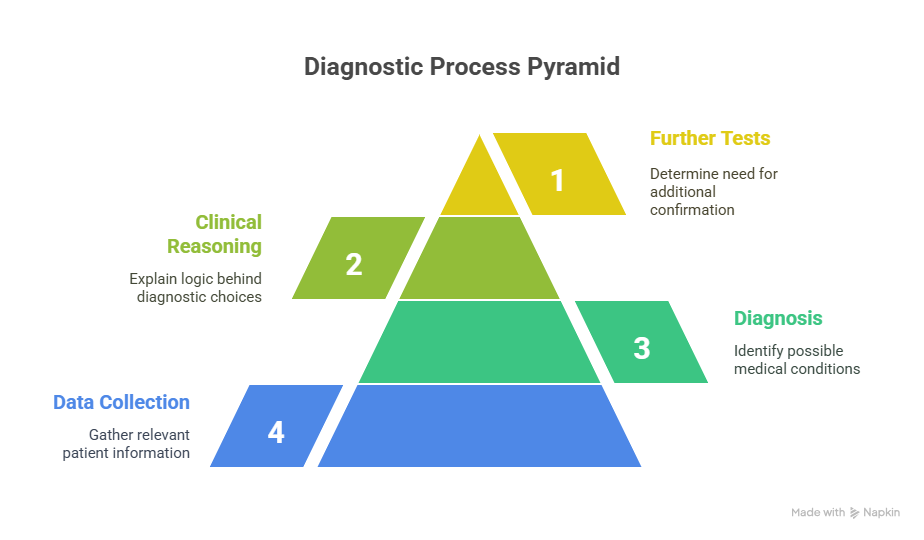
3. State Your Diagnosis or Impressions (Assessment)
Based on the above data, explain:
- Your working diagnosis or list of possible diagnoses
- Clinical reasoning behind your conclusions
- Whether you need further tests to confirm
How Lindy helps:
- Lindy suggests likely diagnoses based on the subjective + objective sections.
- You can dictate your clinical reasoning and Lindy will summarize it into clear, logical text.
- It can even flag uncertainties and recommend additional diagnostics if your template includes that logic.
This section shows your thought process. Be clear, logical, and specific.
4. Outline What Happens Next (Plan)
Lay out your treatment strategy, including:
- Medications or therapies prescribed
- Follow-up instructions
- Referrals or consultations
- Lifestyle or behavior recommendations
How Lindy helps:
- Use a custom plan template or prompt Lindy:
“Lindy, create a treatment plan for mild pancreatitis in a stable patient.”
- Lindy pulls from your previous notes + best practices to draft:
- Clear medication orders
- Follow-up timing
- Patient education notes
- Referral recommendations
Don’t use vague terms like “follow up as needed” or “RTC PRN.”
Be precise. Say exactly what should happen next and when.
With these steps, your SOAP note will be complete, clear, and clinically useful. Whether you're documenting for a busy clinic or prepping for rounds, this format keeps your notes sharp and actionable.
Clinic Note Specifics for Different Healthcare Professions
All clinic notes are not the same. They vary depending on different healthcare professionals.
Here's a deeper look at what SOAP notes tend to emphasize for each specialty:
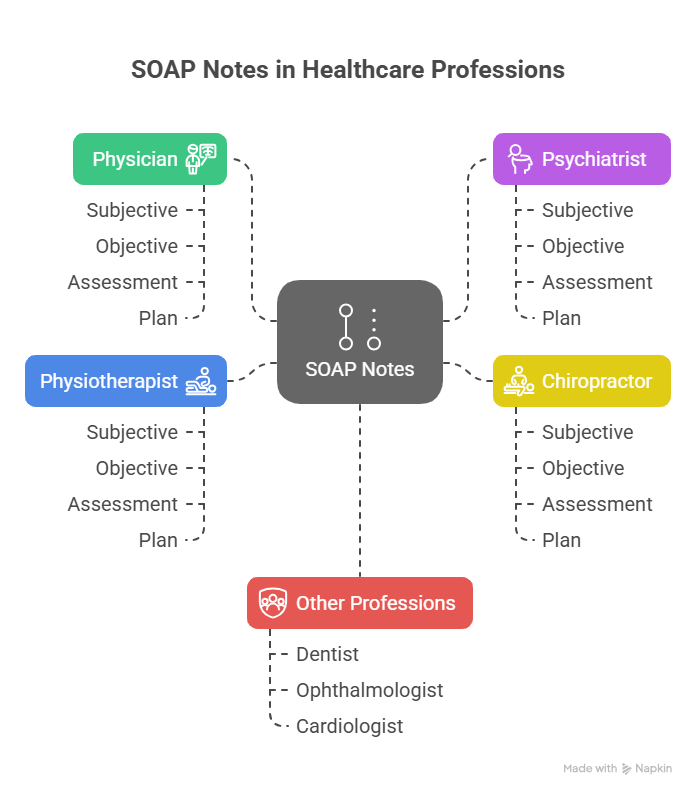
1. Physician:
- Subjective: Chief complaint, history of present illness, relevant medical history, allergies, medications.
- Objective: Vital signs, physical exam findings, relevant lab or imaging results.
- Assessment: Diagnosis or differential diagnoses.
- Plan: Treatment recommendations, including medications, procedures, referrals, and patient education.
2. Psychiatrist:
- Subjective: Patient's self-reported mood, thoughts, behaviors, and any relevant stressors.
- Objective: Mental status exam observations (appearance, affect, speech patterns, thought content).
- Assessment: Diagnosis, including any relevant specifiers (severity, duration).
- Plan: Treatment approach (medication, therapy modalities), safety assessment, and follow-up plans.
3. Chiropractor:
- Subjective: Patient's pain complaints (location, severity, quality), relevant history, aggravating/alleviating factors.
- Objective: Posture assessment, spinal exam (palpation, range of motion), neurological and orthopedic tests.
- Assessment: Diagnosis, subluxations, and other identified musculoskeletal issues.
- Plan: Adjustment techniques, modalities, exercises, and recommendations for self-care.
4. Physiotherapist:
- Subjective: Patient's functional limitations, pain levels, and progress since the previous session.
- Objective: Reassessment of strength, range of motion, functional tests, and pain response to treatment.
- Assessment: Progress assessment, any modifications needed to the treatment plan.
- Plan: Exercise prescription, manual therapy techniques, modalities used, and goals for the next session.
Best Practices for Writing Better Clinic Notes
Even seasoned providers can get bogged down by documentation. But efficient, high-quality notes are possible with a few disciplined practices.
1. Keep It Focused
Don’t document everything. Document what matters. Include only relevant symptoms, findings, and actions tied to the visit’s purpose. Avoid unnecessary narrative. Your goal is clarity, not length.
2. Use Structured Templates
Speed up your workflow by using pre-built templates for common visit types, like annual physicals, chronic condition follow-ups, or medication refills. Templates help standardize documentation and reduce errors. Always personalize based on the patient's presentation.
3. Prioritize Readability
Use consistent headings (SOAP), bullet points for findings, and concise language. This makes it easier for other clinicians to scan and understand your note. Avoid large blocks of text or vague phrasing.
4. Proof Your Work
Typos and copy-paste errors make your notes look careless. Review for accuracy before signing off, especially in the Assessment and Plan. Mistakes in medications, dosages, or diagnoses can lead to serious consequences.
5. Document In Real Time
Whenever possible, complete notes during or immediately after the visit. This improves accuracy and reduces after-hours charting. If delayed, jot key details during the encounter so you’re not relying on memory later.
These best practices will improve both efficiency and clinical quality. They also help keep your notes defensible, readable, and compliant with standards.
How to Speed Up Clinical Notes with Lindy?
Still writing down notes like it’s 1887? Use Lindy as your medical scribe to make clinical notes easy:
- Lightning-fast note creation: Lindy listens intently and transforms your spoken words into 99%+ accurate, detailed clinic notes.
- Effortless EHR integration: With a single click, your notes are uploaded to your EHR (like Epic and Cerner). Lindy syncs up, even pulling in relevant patient data for a complete picture.
- A proactive ally: As you speak, Lindy's AI brain offers helpful suggestions based on your words and the patient's history. Keep what works, customize what doesn't.
- Lindy learns your language: The more you use Lindy, the smarter it gets, adapting to your unique phrasing, abbreviations, and those niche terms you love. Got a thick accent or unique speech pattern? Not a problem.
- Never miss a follow-up: Lindy analyzes those notes and turns them into an actionable task list. It'll give you and your team gentle nudges for follow-ups, tests, referrals, you name it.
- Patient data protection: Security is top of mind. Lindy adheres strictly to HIPAA, PIPEDA, and other privacy regulations, keeping sensitive information under lock and key.
- Reclaim precious hours: Imagine slashing your note-taking time by 80%! That's potentially hours of your day back for what matters most, actually caring for patients.
Try out HIPAA and PIPEDA-compliant AI clinic notes for free.
{{cta}}
Frequently Asked Questions
What’s the difference between SOAP notes and other types of medical documentation?
SOAP notes are a structured method specifically designed for documenting clinical encounters. Unlike narrative or free-form notes, SOAP forces you to organize data into four clear sections: Subjective, Objective, Assessment, and Plan, which improves clarity, continuity, and billing accuracy.
How detailed should each section of a SOAP note be?
Include only what is medically relevant to the current visit. The Subjective section should summarize symptoms and patient concerns concisely. The Objective should list measurable findings. Assessment should be your diagnostic impression, and the Plan must clearly outline next steps. Avoid including unrelated or excessive background.
How do clinic notes differ between specialties like family medicine, psychiatry, or physiotherapy?
Each specialty emphasizes different types of data. For example:
- Psychiatry: Emphasizes mood, thought process, and mental status exam.
- Physiotherapy: Focuses on function, pain scale, and mobility progress.
- Family medicine: Balances chronic disease management, preventive care, and diagnostics. Tailor notes to reflect your discipline's priorities.
Can I use AI to write clinic notes without violating patient privacy?
Yes, but only if the AI tool is HIPAA and PIPEDA-compliant. Tools like Lindy meet these standards and encrypt patient data securely. Always verify compliance before using AI in clinical settings.
What should I do if I fall behind on notes during a busy clinic day?
Use real-time strategies like jotting down quick shorthand during visits. Later, expand into full notes while details are fresh. If you’re consistently falling behind, consider using voice-based AI scribes like Lindy to speed up documentation without sacrificing accuracy.
How can templates help without making my notes feel generic?
Templates reduce repetitive typing for common visits (e.g. diabetes checkups, well-child exams). But you must customize them for each patient’s symptoms, findings, and plan. Think of templates as scaffolding — not a substitute for clinical thinking.
How do clinic notes affect billing and coding accuracy?
Inadequate documentation can lead to underbilling or claim denials. SOAP notes support coding by clearly showing medical necessity, services provided, and level of care. Proper documentation helps ensure reimbursement reflects your work.
What’s the best way to organize notes for a multi-problem visit?
Use subheadings under each SOAP section to separate issues (e.g. "Hypertension" and "Back Pain"). This makes it easier to follow the care plan for each concern and helps billing specialists assign proper CPT codes.
How can I start using Lindy to automate my clinical notes?
Sign up at Lindy’s website and connect your EHR (e.g. Epic, Cerner). You can begin by recording patient encounters with Lindy as your scribe. It transcribes, summarizes, and formats SOAP notes automatically, ready to review and sign. First-time users can try it for free.
What if I use unique clinical abbreviations or have a strong accent — will AI tools like Lindy still work?
Yes. Lindy adapts to your speech patterns, preferred terminology, and clinical shorthand. The more you use it, the smarter it gets. It’s built to handle regional accents and medical-specific language with high accuracy.



















.avif)
.avif)

.png)
%20(1).png)


.png)