Doctors aren’t meant to be data entry machines. Yet EHRs still eat up hours every week.
AI can fix that. It listens, understands, and fills out your notes while you focus on the patient.
In this guide, I’ll show you how to automate EHR data entry with AI, quickly, safely, and without breaking your workflow.
What Is EHR Data Entry Automation?
EHR data entry automation is the use of software (usually powered by AI or rules-based automation) to capture, structure, and input patient information into your Electronic Health Record system without manual typing.
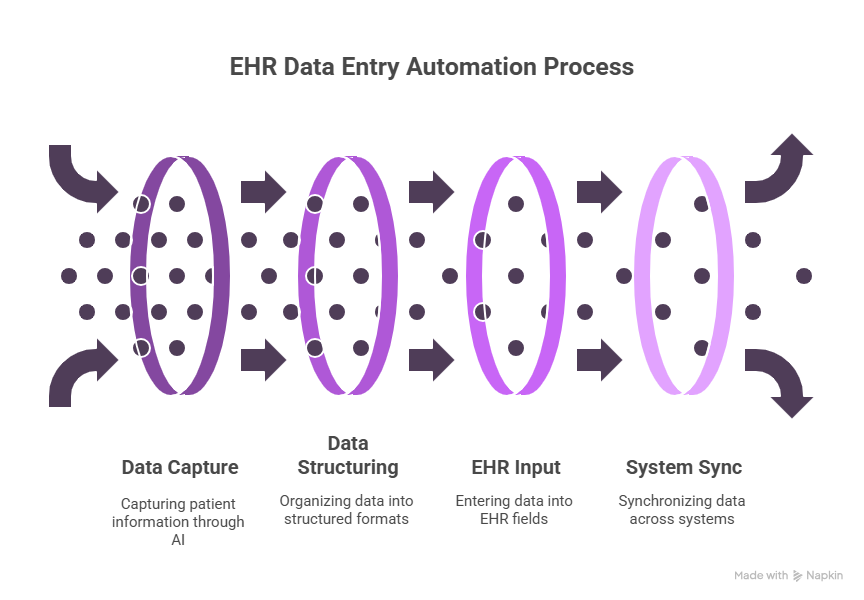
Instead of documenting visits by hand, automation tools:
- Transcribe conversations
- Extract relevant clinical data (like vitals, diagnoses, medications)
- Fill structured EHR fields
- Sync across systems like labs, billing, and scheduling.
How to Automate EHR Data Entry in 5 Steps
Automating your EHR data entry is a phased transformation starting with identifying what slows your team down and building automation workflows one step at a time.
Here’s a complete walkthrough of how to do it right.
Step 1: Map Out Your Manual Workflows and Spot Bottlenecks
Before you automate anything, you need to understand your current process inside out. Start by shadowing clinicians, nurses, and administrative staff during a full patient lifecycle, from intake to documentation to follow-up.
Ask yourself:
- What tasks require the most manual typing or data entry?
- Where is data being repeated across different systems or forms?
- What steps are repetitive and follow the same rules every time?
You’ll likely spot common pain points like:
- Manually transcribing visit notes after each patient
- Copy-pasting vitals, lab results, or imaging summaries into EHRs
- Typing discharge instructions from scratch
- Switching between multiple systems for labs, billing, and scheduling
Your goal in this step is to create a prioritized list of repetitive, rule-based tasks, especially ones that don’t need human judgment. This list becomes your automation roadmap.
Step 2: Choose Tools That Fit Your Workflow, Not the Other Way Around
Once you know what’s slowing you down, it’s time to match each pain point to the right automation solution. Not all tools do the same thing, and not every clinic needs the same stack.
Start by breaking down your needs into three core areas to identify the right tools for your needs:
The right tools will:
- Integrate directly with your EHR (via FHIR, HL7, or native APIs)
- Offer editable, structured outputs, not just raw transcripts
- Include HIPAA compliance and BAA support
- Allow human review before submission
Before committing, ask vendors to demo the exact workflow you want to automate.
Step 3: Build and Roll Out Automation One Workflow at a Time
Trying to automate everything at once is risky and overwhelming. Instead, start small. Pick one high-volume workflow that drains time every day, something like clinical note-taking or vitals entry, and test automation there first.
Here’s a rollout sequence you can try:
1. Start with Clinical Documentation
Use an AI scribe to transcribe real-time patient conversations. Let it auto-generate SOAP notes or visit summaries. Clinicians can then review, edit, and submit the final version to the EHR.
2. Add Structured Data Entry
Once documentation is working well, automate the input of structured fields, like vitals, medications, allergies, or labs. These can be synced directly from monitoring devices, lab platforms, or patient intake forms.
3. Automate Follow-up Workflows
Set up triggers that handle post-visit actions automatically:
- Schedule the next appointment based on diagnosis or provider availability
- Send follow-up instructions or care plans to the patient portal
- Generate billing codes and submit them without manual input
Building your automation layer by layer. That way, each one will be stable before you expand the next.
Step 4: Safeguard Accuracy, Compliance, and Clinical Quality
Healthcare automation doesn’t just need to work, it needs to be safe, secure, and verifiable.
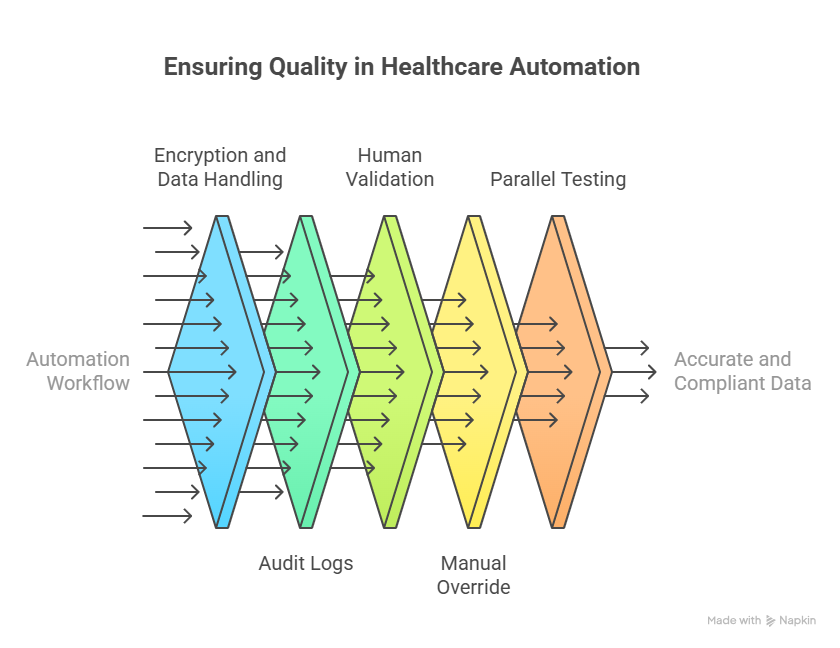
Every automation workflow should have:
- HIPAA-grade encryption and data handling
- Audit logs that track what was automated, when, and by whom
- Human-in-the-loop validation before final data is written to the EHR
- Manual override options in case automation fails or data looks incorrect
Before full rollout, run a parallel test: compare 10–20 patient records generated via automation vs manually completed ones. Look for missing fields, misinterpretations, or incorrect codes.
If your tool generates ICD-10 codes or structured inputs, validate that it's using the latest code sets and referencing correct patient context.
But never use automation to replace clinical judgment. Remove the grunt work, not the decision-making.
Step 5: Train Your Team and Build Confidence in the Process
The best tools will fail if your team doesn’t trust or understand them. Automation adoption is more about people than it is about software.
Here’s how to roll it out smoothly:
- Start with a pilot group. Choose 1–2 tech-friendly clinicians to test the tool in live scenarios and gather feedback.
- Show it in action. Run a live demo that mirrors a real patient visit, showing exactly how the tool listens, transcribes, and pushes structured notes.
- Create training resources. Include SOPs, cheat sheets, and walkthrough videos. Focus on common questions like “How do I fix a wrong entry?” or “Where can I review the draft before submitting?”
- Collect ongoing feedback. Give users a way to flag errors, suggest improvements, or report friction points via a form, Slack channel, or quick survey.
- Celebrate success early. Highlight how many hours were saved, how late-night charting went down, or how clean the records look after automation.
Once your team sees results, they’ll be more open to expanding automation into other parts of the workflow.
What Parts of EHR Data Entry Can Be Automated?
You don’t have to automate everything to get massive time savings. Here are the top areas where automation works best:

1. Clinical Notes & SOAP Documentation: AI scribes can listen to patient visits in real time and generate structured notes (SOAP, H&P, etc.). Some tools even push these notes directly into the EHR.
2. Vitals & Device Data: Vitals from monitors, wearables, or point-of-care devices can be automatically captured and logged in the EHR using integrations.
3. Lab & Imaging Results: Instead of downloading results and manually pasting them, automation can fetch lab reports, extract key findings, and populate the corresponding sections in your EHR.
4. Medication Reconciliation: Tools can cross-check prescriptions, match them to EHR fields, and flag duplicates or conflicts automatically.
5. Appointment Notes & Follow-ups: Post-visit summaries, care instructions, and follow-up reminders can be auto-generated based on visit type and patient condition.
Why Automate EHR Data Entry
Manual data entry eats up valuable clinical time, increases the risk of errors, and adds to staff burnout. Automating this part of your workflow isn’t just a convenience—it’s a strategic upgrade with real impact.
Here’s why it matters:
1. Saves Time for Clinicians
Doctors and nurses often spend 1–2 hours per day just documenting visits, updating fields, or copying information across systems. Automation handles these repetitive tasks in the background, freeing up hours each week that can be spent with patients instead of screens.
2. Reduces Burnout and Administrative Overload
Clerical work is one of the top drivers of physician burnout. When automation handles note-taking, follow-ups, or data syncing, clinicians don’t have to chart late at night or multitask during appointments. The result: more focus, less frustration, and better job satisfaction.
3. Improves Accuracy and Reduces Human Error
Manual entry often leads to typos, skipped fields, or copy-paste mistakes that compromise patient records. Automated systems can consistently extract and input the right data in the correct format, reducing medical errors and the need for costly rework.
4. Scales without Additional Headcount
Whether you're seeing 10 patients a day or 50, automation works at the same pace, without needing to hire more staff. It helps your operations scale smoothly during peak hours, growth phases, or seasonal surges without sacrificing documentation quality.
What You Should Know Before Automating EHR Data Entry
While EHR automation can save you a ton of time, it’s not plug-and-play. There are a few things to keep in mind to make sure your setup is successful and safe.
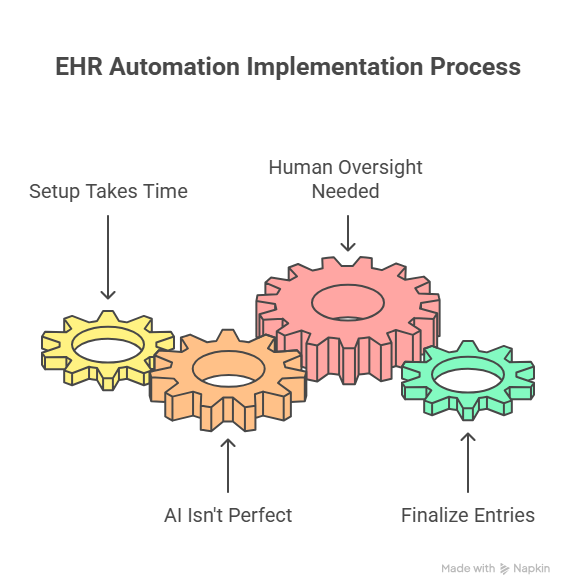
1. Setup Takes Time, Especially for Complex EHRs
Getting automation tools to work with your specific EHR system (like Epic, Cerner, or Athena) may take time, especially if APIs or integrations need to be customized. Expect a bit of IT involvement during implementation, and don’t skip testing in a sandbox environment first.
2. AI Isn’t Perfect with Every Input
Voice-based tools like AI scribes can sometimes misinterpret accents, fast speech, or background noise. If your clinicians don’t speak clearly or if the environment is loud, you might see errors in transcription. Regular quality checks are key to catching these issues early.
3. You Still Need Human Oversight
Automation can handle repetitive tasks, but it can’t replace clinical judgment. Always build a review step into your workflow where a provider double-checks and approves entries before they’re finalized in the EHR. It keeps your data clean and your records safe.
Automation is powerful, but like any tool, it works best when you know its limits and use it with the right safeguards in place.
Skip Manual EHR Data Entry with Lindy
If you're spending hours on documentation, it's time to let AI handle the busywork.
Lindy builds powerful AI agents that automate the entire EHR data entry process, so your team can focus on patients, not paperwork.
Here’s what Lindy can do for you:
- Transcribe patient visits in real time and generate accurate, structured SOAP notes
- Push notes directly into your EHR with one-click review and approval
- Sync labs, vitals, and other third-party data without switching between systems
- Automate follow-up tasks like referrals, discharge summaries, and reminders
- Stay 100% HIPAA-compliant with audit-ready logs and human-in-the-loop workflows
Frequently Asked Questions
1. Can AI do data entry?
Yes, AI can handle data entry by capturing information from voice, text, or forms and inputting it into structured systems like EHRs. It can transcribe conversations, extract relevant details, and auto-fill fields, reducing manual typing, minimizing errors, and significantly saving time for clinical and admin teams.
2. How to automate data entry?
You can automate data entry using AI-powered tools or robotic process automation (RPA). These tools extract information from sources like PDFs, forms, or voice input and input it into systems automatically. Set up integrations or use no-code platforms to define triggers, map data fields, and schedule updates.
3. What is EMR data entry?
Electronic Medical Record data entry (EMR data entry) refers to the manual or automated input of patient data, like vitals, history, medications, and clinical notes, into an EMR system. It’s essential for maintaining accurate patient records, supporting treatment decisions, and enabling billing, reporting, and compliance in clinical workflows.
4. What is medical data entry?
Medical data entry involves recording patient-related information such as demographics, diagnoses, treatments, lab results, and visit notes into digital systems like EHRs or EMRs. It can be done manually by healthcare staff or automated using software to improve accuracy, speed, and data consistency.
5. How can a computer system make documenting orders more efficient?
Computer systems can streamline order documentation by using templates, auto-suggestions, and rule-based logic. They reduce redundant entry, auto-fill medication or lab order details, and flag errors in real time. This speeds up the process, ensures consistency, and improves overall clinical decision-making.
6. How do you automate data extraction in healthcare?
Use AI tools and data integration platforms to pull structured information from documents, voice recordings, or diagnostic devices. These systems can extract key fields like vitals, labs, or ICD codes and send them to EHRs automatically. Integrations via HL7, FHIR, or APIs enable seamless automation.
7. How accurate is AI when it comes to clinical documentation?
AI scribes are highly accurate for structured documentation tasks, especially when trained on medical language. However, occasional transcription errors can occur, especially with accents or background noise, so it’s critical to include a human review step before submission to the EHR.
8. Can automation really handle structured EHR fields, or just notes?
Yes, many tools can extract and auto-fill structured fields like vitals, ICD codes, medications, allergies, and lab values. This goes beyond just generating text summaries; automation can populate the exact EHR sections you’d otherwise fill manually.
9. Is it safe and legal to use AI for EHR automation?
Absolutely, if the tool is HIPAA-compliant, uses encrypted data handling, and offers audit logs. Always confirm that the vendor signs a BAA (Business Associate Agreement) and that your workflows include proper oversight before going live.
10. Will this work with my current EHR system?
Most top automation tools support integration with major EHR platforms like Epic, Cerner, Athena, and eClinicalWorks, either through direct API, FHIR, HL7, or third-party middleware. Always ask the vendor for integration examples or sandbox demos specific to your setup.
11. How much time can I expect to save with automation?
Clinics that implement EHR automation typically report saving 60–90 minutes per clinician per day. That adds up to dozens of hours a month, freeing time for more patient care, less after-hours charting, and a major reduction in documentation fatigue.
12. Do I need to hire developers to set this up?
No. Many AI-powered tools like Lindy offer no-code workflows and visual setup options. You don’t need technical staff to get started, just clear goals, admin access to your EHR, and initial training for your team.
13. What does a typical rollout look like?
Start with a pilot in one department or provider group. Focus on a single workflow, like automating SOAP notes or syncing vitals, and track performance for 2–4 weeks. Once it works reliably, gradually expand to more use cases or teams.
14. How do I make sure the AI isn’t making critical errors?
Build in mandatory review checkpoints. Most tools allow clinicians to preview, edit, and approve AI-generated notes or data before it’s committed to the EHR. You should also run periodic audits to catch edge cases or performance drops.
15. Can I customize what the AI captures or automates?
Yes. Tools like Lindy let you configure what information to extract, how to structure the output (e.g., SOAP, narrative, bullet list), and where that data should land in your system. You can tailor workflows to specialty, provider preference, or use case.
16. How do I get started with Lindy?
Lindy offers a free trial and quick setup. You can build your first AI agent to transcribe visits, generate notes, push to your EHR, and even automate follow-ups, without writing a single line of code. Try Lindy now and eliminate manual data entry from day one.





















.avif)

.avif)
.png)
%20(1).png)


.png)