I’ve tried nearly every medical dictation tool out there, most are clunky, slow, or just plain outdated.
Lindy changed that. It’s fast, accurate, and adapts to how you speak, not the other way around.
In this guide, I’ll share the 5 best medical dictation software tools for 2026, and why Lindy is the one I’d actually recommend to any physician today.
What Is Medical Voice Recognition Software?
Medical voice recognition software, also known as medical dictation software or physician dictation software, is a tool that translates spoken words into written text, specifically for healthcare documentation
For example, if you say “Type 2 diabetes with peripheral neuropathy,” the software knows exactly what you mean and writes it out correctly without needing to repeat or correct it.
Unlike general speech-to-text apps, voice-to-text medical tools follow healthcare standards, including HIPAA compliance, and often format your notes based on how doctors work.
Some medical speech-to-text software also supports voice commands, so you can insert common phrases or move through templates with your voice.
In short, it’s a faster, safer way to handle clinical documentation and a valuable tool for reducing admin work in your day.
5 Best Medical Speech Recognition Software
- Lindy: Best for automated SOAP notes
- DeepScribe: Best for real-time medical scribing
- Dragon Medical One: Best for voice-first clinical documentation
- Amazon Transcribe Medical: Best for scalable medical transcription
- Notta: Best for multilingual AI note-taking
Common Terms in Medical Dictation Software
1. Lindy: Best for automated SOAP notes
What does it do? Lindy is an AI-assisted dictation software for medical professionals that listens to patient interactions, transcribes them in real time, and creates structured clinical documentation.
Who is it for? Best for doctors who want to cut charting time and automate admin tasks, especially those using Epic, Cerner, or other major EMR platforms.
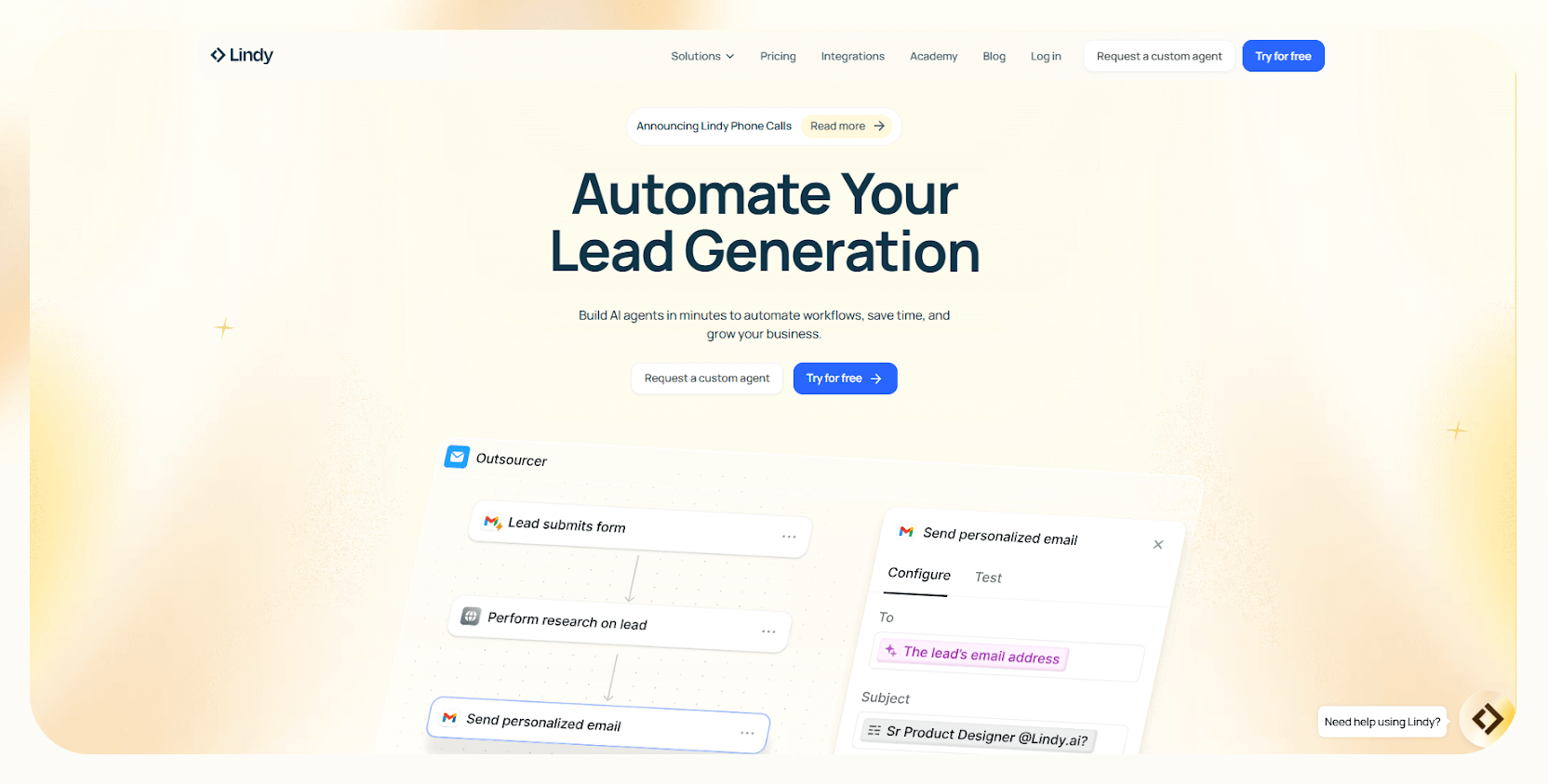
Lindy listens to your patient conversations and automatically formats everything into structured SOAP notes, referral letters, or billing documentation, without you lifting a finger.
The interface is clean and intuitive, no commands to memorize, no need to adjust how you work.
What sets Lindy apart is how it connects medical voice recognition software with your EHR. Once the consultation is over, your notes are already where they need to be. No templates to click through, no empty fields to fill, just a ready-to-sign chart that reflects your voice and documentation style.
And Lindy learns your speech patterns and documentation preferences, meaning fewer corrections over time. You’ll even start seeing smart suggestions for follow-ups, next steps, and tasks you might have otherwise forgotten, especially useful for high-volume days.
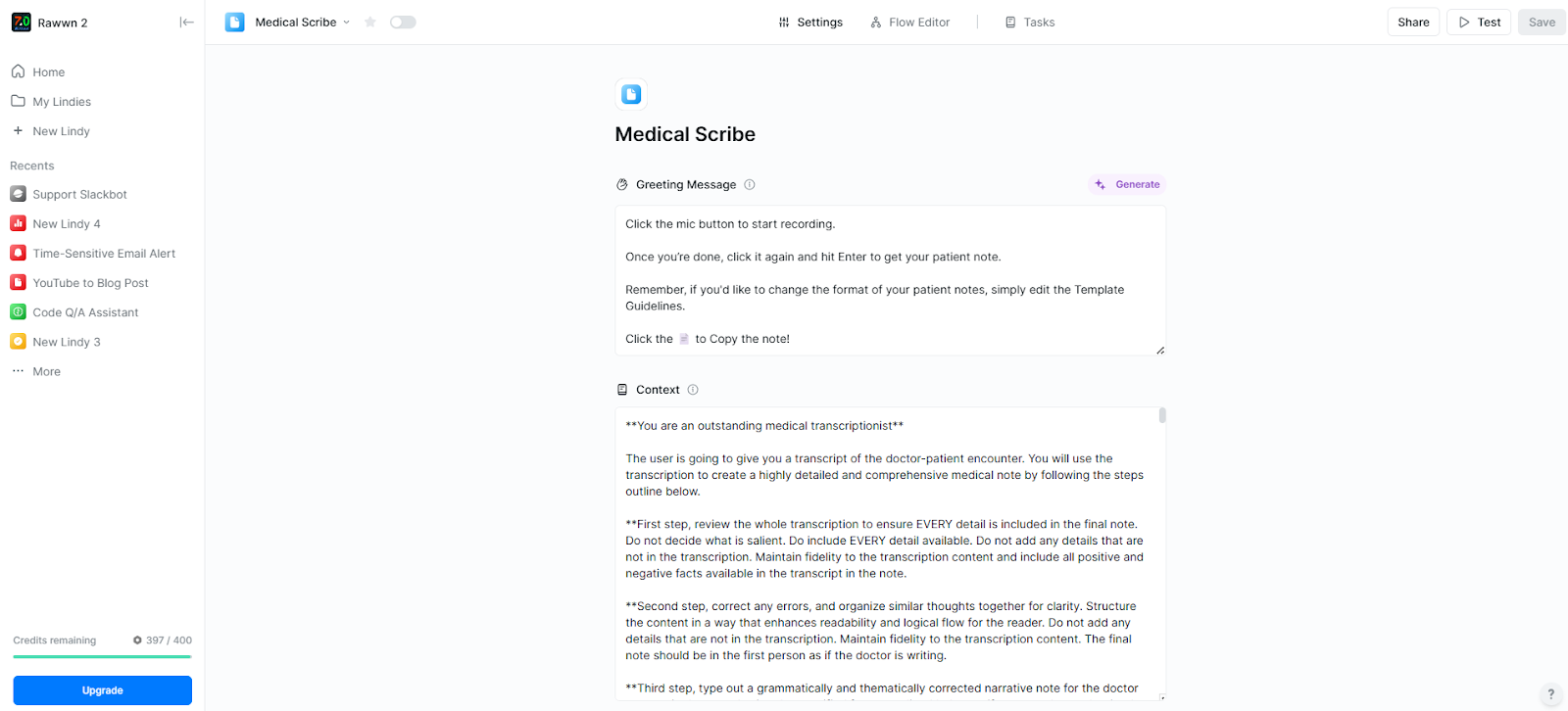
Beyond dictation, Lindy helps you cut down on admin entirely. You can automate repetitive workflows like scheduling, reminders, and cancellations. For busy clinics and solo providers alike, it’s a huge time-saver.
Lindy is fully HIPAA-compliant, so your patient data stays secure, and your mind stays at ease. Plus, you can also switch between AI models and give Lindy memory, so it adapts to how you speak, remembers your workflows, and supports ongoing documentation tasks.
Pros
- Lindy Academy to get familiar with and get quick support
- Significantly cheaper than hiring a full-time medical scribe
- Fast to set up and doesn’t require tech support or a long onboarding process
- Offers a free trial with real features, allowing full evaluation before committing
- Works well even when switching between multiple EMR systems or virtual platforms
Cons
- Best performance relies on a consistent mic/audio environment
- Some advanced EMR features may require a custom setup to integrate fully
Pricing
- Free Plan: 400 credits per month, allowing up to 400 tasks, a knowledge base of up to 1 million characters, and providing access to over 100 integrations.
- Pro Plan ($49.99/month): 3,250 credits monthly, supporting up to 50,000 tasks, 30 phone calls per month, a knowledge base capacity of up to 20 million characters, and access to over 4,000 integrations.
- Business Plan ($299.99/month): 15,000 credits monthly, unlimited phone calls in over 30 languages, priority support, and expands the knowledge base capacity to 50 million characters.
{{templates}}
2. DeepScribe: Best for real-time medical scribing
What does it do? DeepScribe is an AI medical scribe that listens during patient visits and automatically creates clinical notes in real time.
Who is it for? Ideal for primary care providers and specialists who want to reduce after-hours charting and eliminate manual documentation.
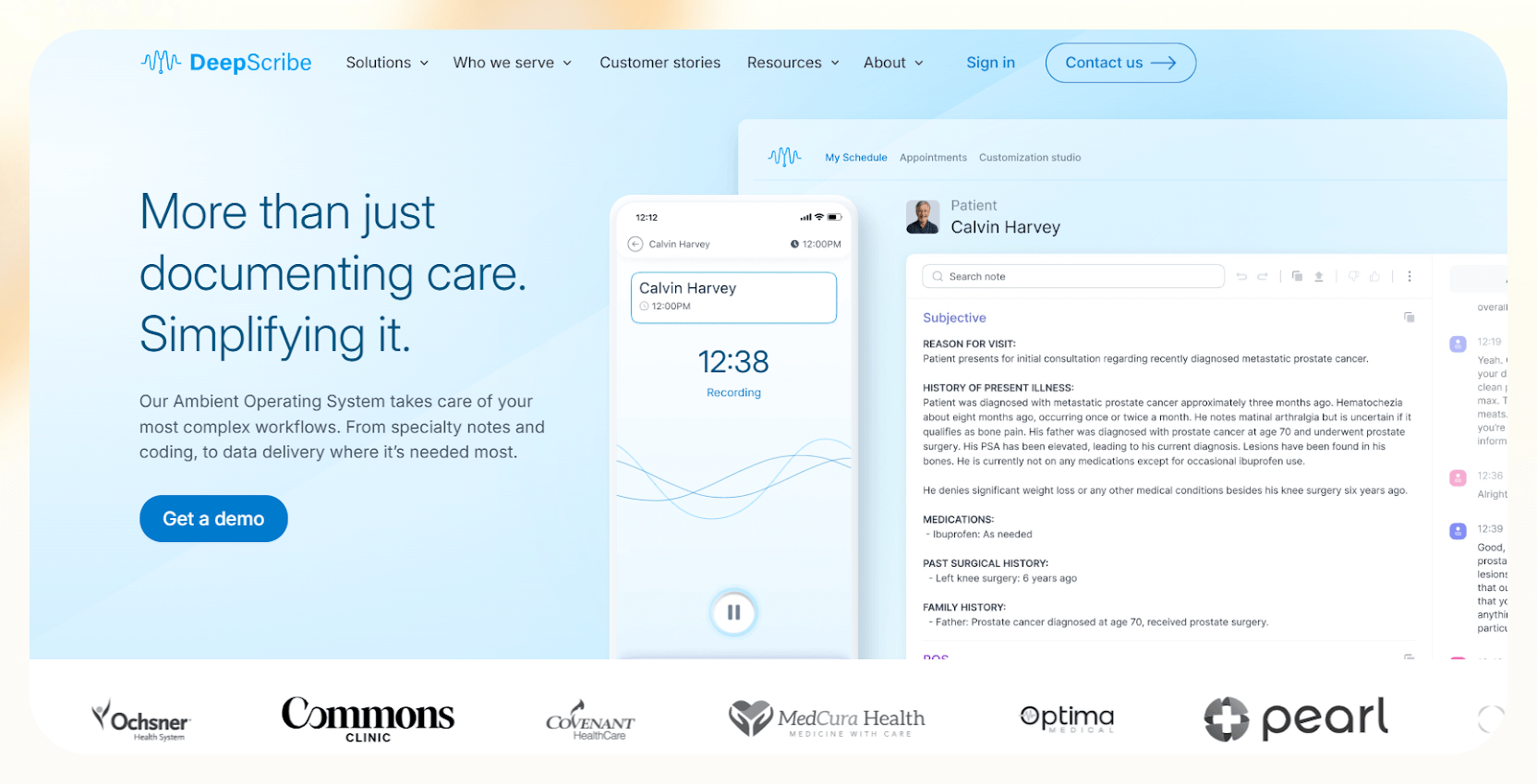
I’ve used DeepScribe during patient visits, and the difference it makes is immediate. You just start talking naturally to the patient, and the software quietly builds your notes in the background.
You do not need to pause, give commands, or repeat yourself. It understands medical language really well, even when you’re explaining things in plain terms.
You can change how your notes are written, from sentence style to note structure, with the customization studio. It doesn’t feel robotic or generic; it actually sounds like you wrote it.
The new E/M coding feature helps you save some time as it listens to the visit and recommends billing codes automatically, including ICD-10, so you don’t have to remember or look them up later. Not to forget, this also helps reduce billing errors.
The EHR integration is smooth. After finishing the appointment, there’s no copy-pasting or downloading. Everything’s already where it needs to be.
And if you work in a specific specialty, the templates adapt to your needs, which makes the documentation even more accurate. To test things, you can also opt for a demo, and the experts will walk you through the platform.
Pros
- Hands-free experience, no commands or manual formatting needed
- Built-in safety and trust features improve transparency with AI-generated content
- Frequent software updates make the tool feel fresher and more accurate over time
- “Clinical Moments” lets you trace notes back to exact parts of the conversation
Cons
- Doesn’t work well in noisy environments or with multiple people talking at once
- You still need to double-check the AI’s note before signing off, especially for complex visits
Pricing
DeepScribe doesn’t list pricing publicly. You’ll need to schedule a demo and get a quote based on your practice size and EHR system.
3. Dragon Medical One: Best for voice-first clinical documentation
What does it do? Dragon Medical One is a cloud-based medical speech-to-text software that lets doctors create accurate, secure clinical documentation using just their voice.
Who is it for? Built for healthcare professionals who need fast, hands-free, and accurate documentation across hospitals, multi-location practices, or while moving between workstations.
After using Dragon Medical One in both hospital and clinic settings, I realized how fast and reliable it is. You don’t need to train your voice or set up profiles. Just log in and start dictating.
Whether you’re using a desktop or a laptop, it picks up your voice clearly and types almost as fast as you talk.
The thing that I found incredibly helpful is the ability to create voice commands. You can set up shortcuts for common phrases, templates, or navigation tasks in your EHR. Saying “Insert physical exam template” and having the whole section drop in perfectly saves a lot of time.
It also includes a PowerMic Mobile app. You don’t need to carry an extra mic as your phone becomes your microphone. That makes it secure and responsive.
Also, this medical voice recognition software is designed with privacy in mind. It’s HIPAA-compliant and cloud-based, so everything you dictate is encrypted and secure. Though it’s easier to use on a Windows setup, the tool is nevertheless packed with advanced features.
And because the license is tied to the user (not the device), you can move freely between workstations without losing your setup.
Pros
- Works smoothly across multiple devices with one login
- Accurate even with regional accents or background chatter
- Custom voice commands let you automate daily workflows
- Excellent support, plus fast onboarding with a Nuance-certified expert
Cons
- Works only on Windows-based devices
- Slight delay when switching devices or network connections
Pricing
Dragon Medical One starts at $99/month for a 1-year plan.
4. Amazon Transcribe Medical: Best for scalable medical transcription
What does it do? Amazon Transcribe Medical is a cloud-based speech-to-text medical transcription tool that converts medical speech into accurate text, either live or from audio files.
Who is it for? Ideal for healthcare teams, telehealth providers, researchers, and developers who need a scalable, affordable, and highly customizable transcription tool.
Amazon Transcribe Medical does a solid job of picking up medical language. You don’t have to teach it much. It already knows clinical terms, drug names, as well as abbreviations.
You can use it to transcribe live audio while talking to a patient or upload files in bulk if you’re dealing with interviews, research recordings, or multi-person consultations. It handles one-on-one and some multi-speaker scenarios reasonably well, though background noise can impact accuracy.
There is also a custom vocabulary. You can add your own terms or uncommon phrases. This helped a lot when I had to transcribe notes in more niche medical contexts.
And because it’s part of AWS, it’s easy to connect it with tools like Amazon Comprehend Medical to extract conditions, medications, or diagnoses from the text.
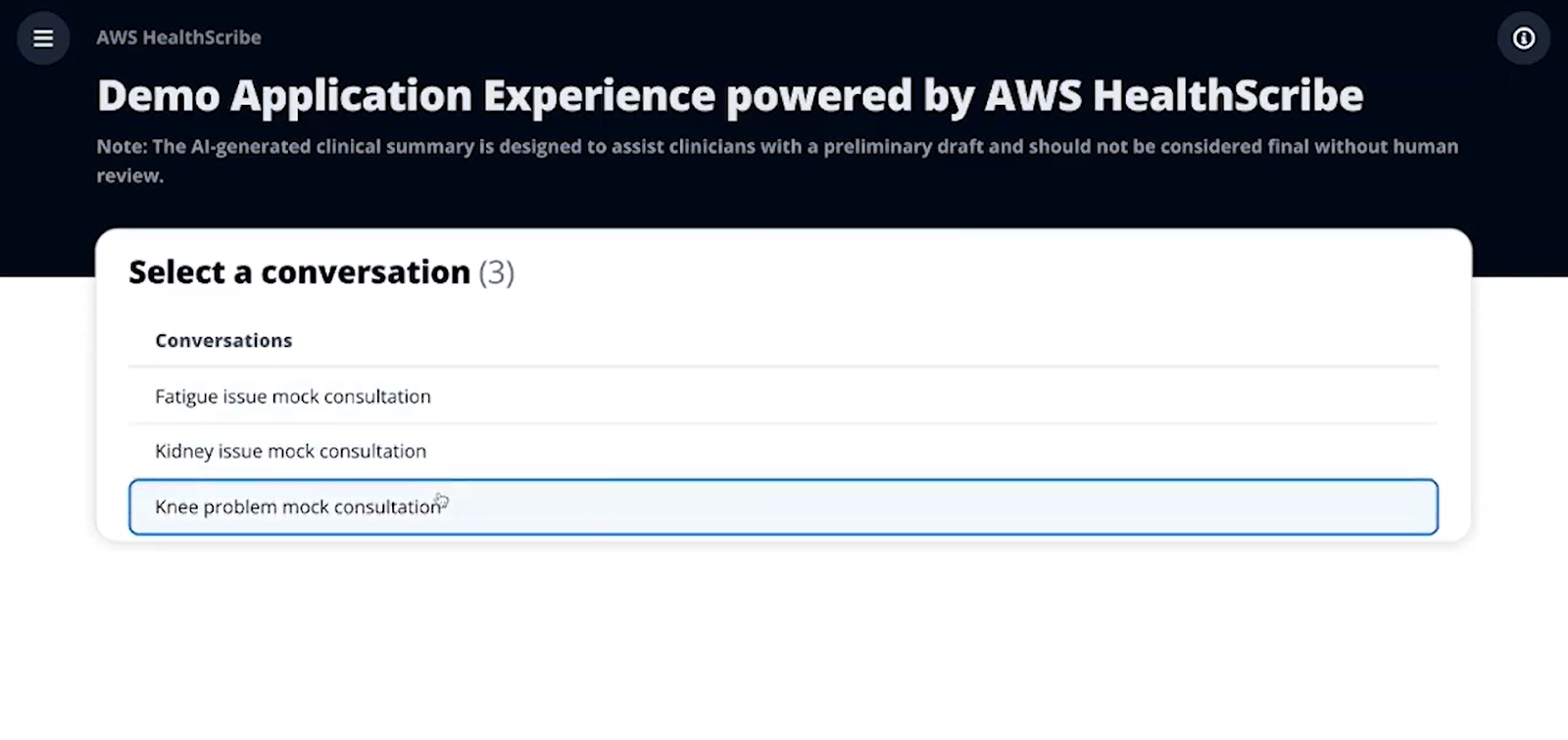
When it comes to security, it’s HIPAA-eligible and doesn’t store your data unless you choose to. That gave me peace of mind when handling patient conversations.
Plus, there are no upfront costs. You just pay for what you transcribe, which keeps it budget-friendly, especially for teams or projects that don’t have a consistent volume.
Pros
- Supports both real-time and batch transcription
- Recognizes multiple speakers accurately in one conversation
- Enables phonetic search within transcripts for quick term lookup
- Offers specialty-specific tuning for fields like cardiology and neurology
Cons
- Requires technical setup
- Only supports U.S. English for medical transcription
Pricing
- Free Tier: 60 minutes per month for the first 12 months after signup.
- Standard Pricing (Pay-as-you-go): You are billed based on the seconds of audio transcribed per month, with usage billed in one-second increments (minimum 15 seconds per request).
Example pricing for the US East (N. Virginia) region:
- 15 minutes: $1.125
- 30 minutes: $2.250
- 45 minutes: $3.375
- 60 minutes: $4.500
- 75 minutes: $5.625
- 90 minutes: $6.750
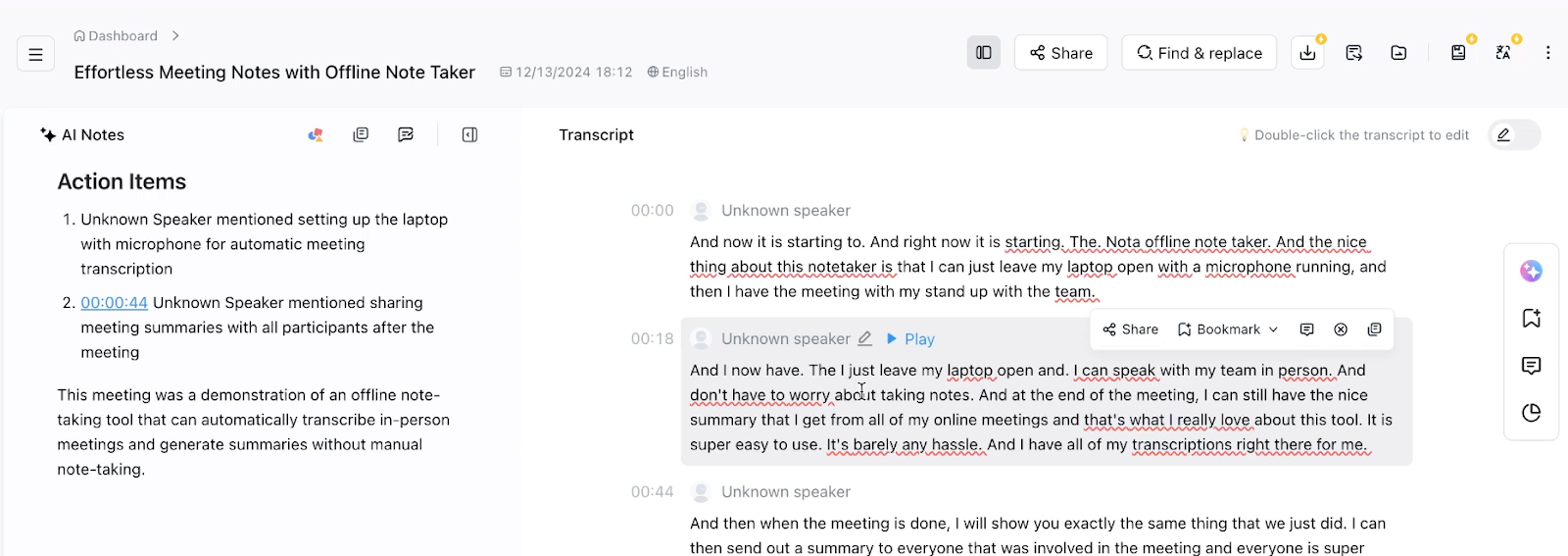
5. Notta: Best for multilingual AI note-taking
What does it do? Notta is a transcription and meeting assistant powered by AI that transcribes live audio, summarizes conversations, and translates transcripts into multiple languages.
Who is it for? Perfect for medical professionals, researchers, and support teams who need multilingual transcription, easy meeting summaries, and tools to share, edit, and store transcripts securely.
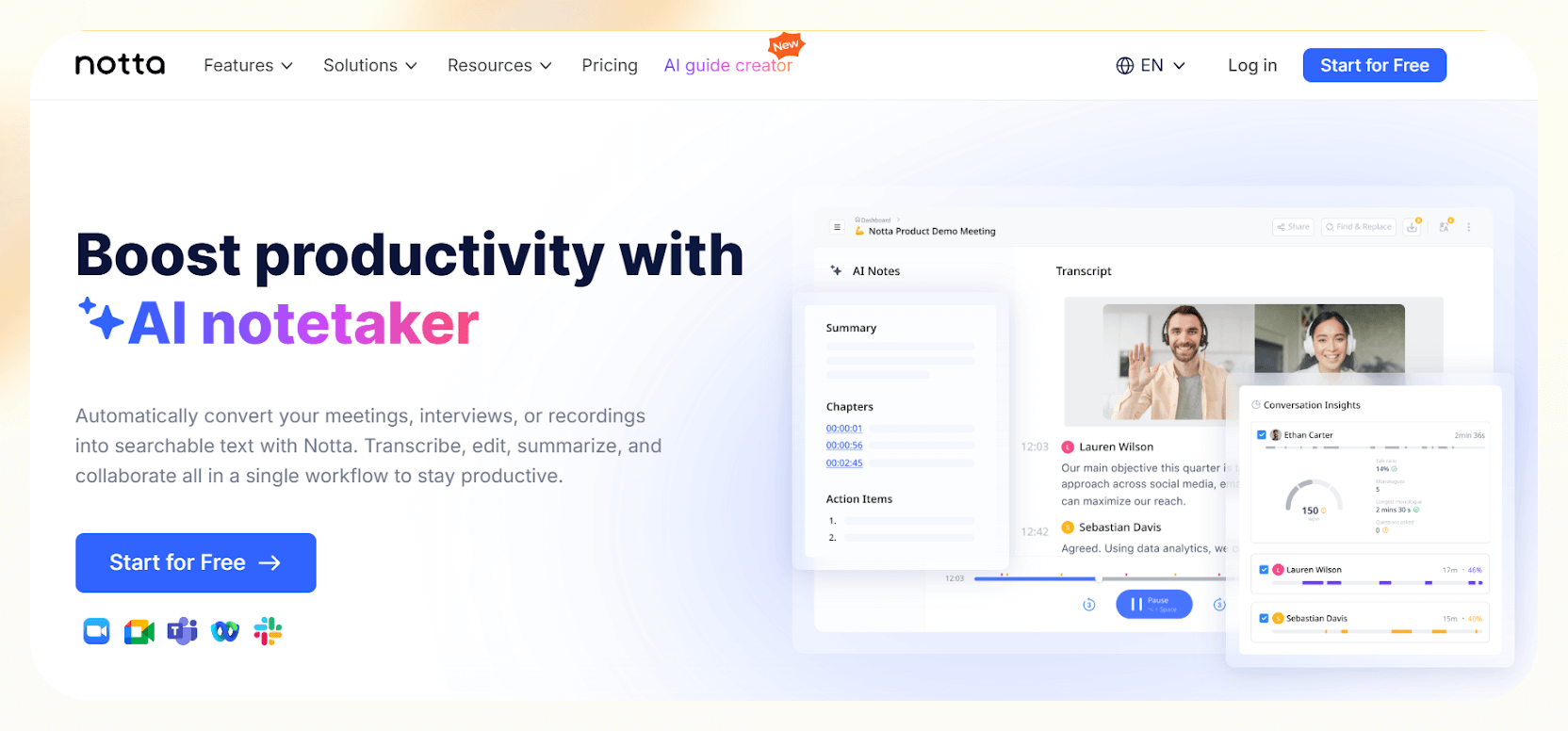
Using Notta feels less like using a transcription app and more like having a smart assistant that listens with medical speech recognition software, takes notes, and organizes everything for you. I’ve tested it during virtual meetings, and it picks up conversations clearly, even with multiple speakers or a mix of languages.
The AI summary tool is one of my favorite features. After a session, it doesn’t just give you a transcript, it highlights action items, decisions, and key points. This saves time if you need a quick overview for reports or follow-ups.
The integrations with Zoom, Google Meet, Microsoft Teams, and even Google Calendar make things easier. You can set it up to join meetings automatically, record, transcribe, and summarize.
You can edit transcripts, and you can export them in all the major formats (DOCX, TXT, PDF, XLSX, and even SRT for subtitles). It also supports real-time collaboration, so you and your team can co-edit transcripts and leave comments, just like in Google Docs.
Security-wise, it’s enterprise-grade, with certifications like SOC 2 Type II and ISO 27001, which is reassuring if you’re handling sensitive medical discussions.
Pros
- Semantic segmentation makes transcripts easier to follow and review
- Playback speed controls and noise reduction enhance review quality
- Built-in translation and export tools make it great for international workflows
- Bilingual and multilingual transcription with speaker identification is incredibly accurate
Cons
- Not built specifically for healthcare, no native medical vocabulary support
- AI summaries are helpful, but may miss finer clinical details if not reviewed
Pricing
- Free Plan: 120 transcription minutes/month, 3-minute max per recording, 50 file uploads/month, 10 AI summaries/month
- Pro Plan ($8.17/month): 1,800 transcription minutes/month, 90-minute max per recording, 100 file uploads/month, 30 AI summaries/month
- Business Plan ($16.67/month): Unlimited transcription, 5-hour max per recording, 200 file uploads/month, 50 AI summaries/month
How I Tested the Best Speech-to-Text Medical Transcription Tools
To create this list of speech-to-text medical software, I didn’t just rely on marketing claims or feature pages. I spent time using each of these tools in real-world clinical scenarios, whether it was during simulated patient consultations, follow-up note dictation, or testing integrations with EHR systems.
Here’s what I specifically looked at:
- Accuracy in real use: Each tool was tested on how well it recognized medical terminology, complex diagnoses, drug names, and common abbreviations. I used both casual and clinical sentence structures to gauge adaptability. Accent handling, background noise, interruptions, and the frequency of manual corrections were also part of the review.
- Speed and responsiveness: Real-time transcription speed was a key factor. The focus was on how quickly spoken words were converted to text, especially during fast-paced consultations. Any lag that could disrupt documentation flow or affect patient focus was noted.
- Ease of use: I assessed how easy each tool was to set up and start using. This included how long it took to install, whether it needed voice training, and how intuitive the interface was. I also considered how easily it fit into my existing workflow, without forcing me to adapt or change how I typically work.
- EHR integration: I tested how well the software connected with electronic medical record (EMR/EHR) systems, especially common platforms like Epic, Cerner, and athenahealth. I looked at whether notes were automatically added to the right sections or whether I had to copy, paste, or reformat them manually, which would defeat the purpose of automation.
- Custom features: Features like voice commands, pre-set templates, SOAP note automation, ICD-10 suggestions, and AI summaries were examined not just for existence, but for how helpful they were in actual workflows.
- Security and compliance: Since these tools deal with sensitive patient data, I verified whether each one was HIPAA-compliant. I also looked at how data was stored, whether it was encrypted, and if users had control over where and how their data was handled. Tools that lacked transparency or defaulted to cloud storage without an opt-out were marked down.
- Value for money: Pricing was assessed with what each tool delivered. Flexibility in plans, essential features behind paywalls, and how each option compared to hiring a scribe were key factors. Trial availability and refund policies were also considered.
Each tool was tested from a clinician’s point of view, with an emphasis on reducing charting time, improving note accuracy, and cutting down on admin fatigue. Only those that performed consistently well across all categories made the final list.
{{cta}}
How Can Lindy Help?
Lindy isn’t just a medical dictation tool, it’s your AI teammate. You can use it to:
- Transcribe patient interactions
- Generate SOAP notes
- Automate admin tasks, like scheduling and reminders
But what makes Lindy stand out is how flexible it is.
You’re not locked into one workflow or model. You can switch between AI models based on what works best for you, and even give your AI “memory”, so it learns your preferences, adapts to your style, and helps with ongoing tasks across different patients or clinics.
Whether you’re working solo or managing a care team, Lindy can act as a smart assistant that evolves with your practice. Try it out and see how much time and mental load it can take off your plate.
Explore Lindy’s AI Healthcare Assistant→
Frequently Asked Questions
1. What’s the difference between medical dictation and regular voice recognition software?
Medical dictation software is made for doctors and healthcare professionals. It understands medical terms like “hypertension” or “bronchoscopy” and knows how to format patient notes correctly. Regular voice software, like Google Voice or Siri, can’t understand these complex terms and often makes mistakes in medical writing.
2. Is medical speech recognition software HIPAA-compliant?
Yes, most medical dictation tools are built to follow HIPAA rules. This means they keep patient data private and secure. Still, it’s smart to double-check the software’s privacy policy and make sure it says it is HIPAA-compliant before you start using it.
3. Do I need special equipment to use medical dictation software?
No, you don’t. You can use your regular computer and a good microphone. Some tools even let you use your smartphone as a mic. Since many of these tools are cloud-based, you don’t need to install anything complicated.
4. How accurate is medical speech-to-text software today?
Very accurate. The best software today can understand medical language with up to 99% accuracy. It also learns your voice, accent, and speaking style over time, so it gets better the more you use it.
5. Is there free dictation software for medical professionals?
Yes, you can try free software, but these tools don’t have medical vocabulary or security features. They might work for simple notes, but they’re not safe or accurate enough for real patient records. For professional use, it’s better to choose a tool made for healthcare.
6. How do these tools understand different accents or languages?
Good dictation software uses AI to learn your voice and accent. The more you use it, the better it gets. Some tools also support other languages or bilingual speakers, which is helpful in hospitals with diverse staff and patients.
7. What’s the best dictation software for solo doctors or small clinics?
Lindy is one of the best dictation software programs for solo doctors or small clinics, especially if you’re looking for something easy and affordable. Other tools like Notta or DeepScribe are also simple to set up. They don’t need IT support and offer flexible pricing, too.
8. How does AI help with medical transcription?
AI significantly enhances medical transcription by automating and improving the accuracy of the process. AI systems use advanced speech recognition and natural language processing to understand and transcribe spoken medical language, reducing human error and saving time.
9. Can I connect dictation software to my EHR system?
Yes, many medical dictation tools work with popular EHR systems like Epic or Cerner. This lets you speak directly into the patient’s chart without switching windows. Just check whether the software supports your EHR before you buy.
10. Is it hard to learn how to use medical dictation software?
Not really. Learning to use medical dictation software can involve a learning curve, particularly as it requires a new way of writing by speaking. However, once you're comfortable with the process, it can significantly streamline your documentation and improve accuracy.



















.avif)
.avif)
.png)
%20(1).png)



.png)